Psychedelics show great promise as a breakthrough treatment for depression, but their use in treating bipolar depression—particularly bipolar I disorder—raises some significant concerns. Psychedelics can produce effects similar to mania, and there have been reports of individuals experiencing mania after using psychedelics recreationally.
However, if used intentionally within a controlled, therapeutic setting, could the promises outweigh the risks?
Key Takeaways
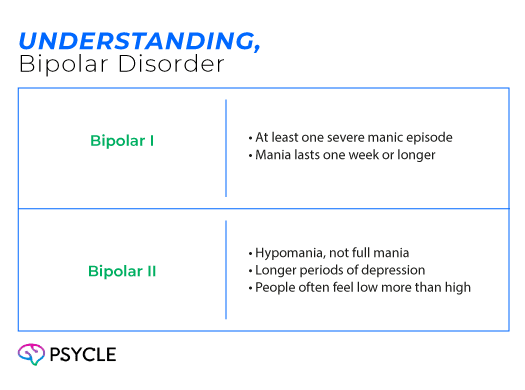
- Bipolar disorder involves cycles of mania/hypomania and depression, with bipolar I having severe mania and bipolar II featuring longer depressive periods.
- Conventional medications can help but often cause side effects and require trial-and-error, leading to interest in new treatments like psychedelics.
- Psychedelic-assisted therapy (PAT) combines supervised psychedelic use with therapy.
- Small studies suggest PAT can reduce depressive symptoms and improve quality of life in bipolar II.
- Psychedelics can trigger mania, especially in bipolar I, while ketamine may be a safer alternative.
Understanding Bipolar Disorder
People with bipolar disorder move between episodes of mania, or hypomania, and depression. These emotional states affect someone’s mood, energy, and ability to function.
A manic episode is characterized by persistent high energy, increased risky and impulsive behaviours, and uncontrollable racing thoughts. Hypomania is similar, but the symptoms are less intense and the episodes are shorter.
Depression, on the other hand, is characterized by persistent low mood and a loss of interest in activities.
Bipolar disorder appears in one of two forms. Bipolar I includes at least one severe manic episode that lasts a week or longer. Bipolar II involves hypomania and more extended periods of depression. People with bipolar II often spend more time feeling low than high.
Treatment for bipolar disorder typically includes a combination of psychotherapy, lifestyle management, and medication. Someone’s medication regimen will vary depending on their condition, but common drugs include:
- Mood Stabilizers: Help control mood swings and prevent episodes of mania and depression, e.g., lithium
- Anticonvulsants: Originally developed for epilepsy, these also help regulate mood and reduce the intensity of manic and depressive episodes, e.g., lamotrigine
- Atypical Antipsychotics: Used to manage mania, psychosis, and bipolar depression, and to maintain long-term mood stability, e.g., quetiapine
- Antidepressants: Sometimes prescribed for bipolar depression but used cautiously, as they can trigger manic episodes, e.g., fluoxetine
Bipolar medications can help, but they have challenges. They can cause unpleasant side effects like weight gain, sleepiness, and memory problems. Finding the right combination also often takes a lot of trial and error, which can be discouraging for people.
For these reasons, there’s a growing interest in innovative therapies for treating bipolar. Research studies suggest psychedelics could be a promising solution.
What is Psychedelic-Assisted Therapy
Psychedelic-assisted therapy (PAT) involves a combination of therapeutic sessions with psychedelic drugs, such as psilocybin (the active ingredient in magic mushrooms), MDMA, and ketamine. These substances cause changes in the brain that affect how people think and perceive. PAT harnesses these effects to help people break free of unhealthy thinking and behaviour patterns.
A typical PAT session has three parts:
- Preparation: You meet with a therapist to set goals and discuss what to expect.
- Dosing: You take the psychedelic under supervision in a calm, safe space.
- Integration: After the session, you discuss what you experienced and how to apply it to your daily life.
Most PAT so far has been limited to research settings. However, multiple studies have shown that this form of therapy has significant long-lasting benefits for various mood disorders, including depression and anxiety.
In recent years, some regions have started permitting legal psychedelic-assisted therapy (PAT) under specific conditions. For example, in Australia, psilocybin-assisted therapy is available for people with treatment-resistant depression (TRD). In Oregon, psilocybin can be used for therapy at specially licensed facilities.
Potential Benefits of Psychedelic-Assisted Therapy for Bipolar Disorder
Several studies have shown that PAT can effectively treat depression, even in people who haven’t responded to conventional medications. This raises the possibility that it could also benefit individuals with bipolar depression, particularly type two, where depression is more prevalent.
In an open-label trial, 15 adults with bipolar II depression received a single dose of psilocybin alongside psychotherapy. Three weeks after treatment, all participants showed a significant reduction in depression scores and an improvement in quality of life. Twelve participants experienced a symptom reduction of more than 50%, and 11 were considered in remission.
The study also suggested that psychedelic therapy was safe for people with bipolar II, as no participants showed increases in mania during the trial. However, there was only a small sample size, so more research is needed.
The Link Between Psychedelics and Mania
A major concern when it comes to psychedelics and bipolar disorder is that these substances could trigger manic or psychotic episodes. The risk is more relevant for people with bipolar I, who have a history of full manic episodes.
Classical psychedelics work by acting on serotonin, a chemical messenger in the brain that plays a role in mood and sleep. Overactivation of the serotonin system may contribute to mania, since antidepressants–which also act on serotonin–can trigger manic episodes in people with bipolar disorder.
As such, even though psychedelics may relieve depression in people with bipolar, they could destabalize someone and trigger a manic episode. There have been several case reports of people having manic episodes after using psychedelics, highlighting this risk.
One web-based surveyinvestigated the link between psilocybin use and changed symptoms. The study included 541 people with bipolar types one and two who used psilocybin, mostly in the form of magic mushrooms.
About one-third reported new or increased symptoms, most commonly manic symptoms, sleep difficulties, and anxiety. However, despite these effects, most participants reported that psilocybin was more helpful than harmful.
Currently, people with bipolar II are mostly excluded from psychedelic clinical trials. Yet, researchers are currently investigating whether the therapy could be safe when given in carefully controlled clinical environments.
Ketamine Therapy for Bipolar Disorder
Ketamine is sometimes classed as a psychedelic because it changes perception and consciousness. It also has significant benefits in treating depression and other mental health disorders. However, it works differently to classical psychedelics as it acts on the chemical messenger glutamate, instead of serotonin.
Because of this difference in action, ketamine is thought to be less risky when it comes to treating bipolar disorder. Clinics may offer ketamine treatment to people with the condition on a case-by-case basis.
In an observational study, 66 people with treatment-resistant bipolar I or II depression received four low-dose IV ketamine infusions over two weeks. The treatment led to significant improvements in depression, anxiety, suicidal thoughts, and daily functioning. The infusions were generally well tolerated, with only three patients reporting mild hypomania and no reports of full mania or psychosis.
FAQs
Can Psychedelics Help Prevent Future Depressive Episodes in Bipolar Disorder?
Current research has focused treating active depression rather than prevention. However, PAT may help patients develop new coping mechanisms and mental frameworks, which could indirectly reduce relapse risk. Long-term studies are still needed.
Can I Enter a Psychedelic Clinical Trial if I Have a History of Mania?
Most clinical research studies using psychedelics exclude people who have a history of mania, or family history of manic and psychotic disorders. However, as research develops, carefully controlled studies may accept patients with these risks.
Sources
- https://www.sciencedirect.com/science/article/abs/pii/S0165032724020317
- https://journalbipolardisorders.springeropen.com/articles/10.1186/s40345-022-00265-5
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10296406/

