Cognitive Behavioral Therapy (CBT) is one of the most widely used and well-studied forms of psychotherapy. It focuses on how thoughts, emotions, and behaviors interact, and how small, deliberate changes in one area can have a positive impact on overall mental health. CBT has proven effective for conditions such as depression, anxiety, post-traumatic stress disorder (PTSD), and insomnia, and it continues to evolve as research expands.
This article explores what CBT is, how it works, and why it remains a cornerstone of modern mental health care. It also looks at emerging applications, including how CBT is increasingly paired with psychedelic-assisted therapies to help people process insights and sustain positive change after treatment.
Key Takeaways
- CBT links thoughts, feelings, and behaviors; shifting one element can shift the rest.
- This is a practical, structured, and skill-based approach, typically offered in a short-term format.
- CBT can be used for depression, anxiety, trauma, insomnia, and more.
- Cognitive Behavioural Therapy is evidence-based and adaptable for many people.
- CBT focuses on realistic, not just positive, thinking.
- People integrating insights from psychedelic therapy are finding CBT helpful.
CBT: Origin Story
Cognitive Behavioral Therapy grew from two earlier approaches: behaviorism, which focused on how actions are learned and repeated, and cognitive therapy, which explored how thoughts shape feelings.
In the 1960s, psychiatrist Aaron T. Beck noticed that many of his patients’ emotional struggles were tied to habitual, automatic thoughts. He developed structured ways to question and change those patterns, and CBT was born.
Since then, CBT has become one of the most researched and widely practiced forms of psychotherapy in the world. It’s used in hospitals, clinics, private practices, and increasingly, online.
But at its heart, it still revolves around one simple, powerful idea: change your thinking, and your emotional world can begin to change too.
A Goal-Oriented Talk Therapy
CBT is a structured, goal-oriented form of talk therapy that helps you identify unhelpful patterns in your thoughts and actions and replace them with more balanced, realistic ones.
“Cognitive” refers to what happens in your mind — the stream of interpretations, beliefs, and mental shortcuts that shape how you see the world. “Behavioral” refers to what you do in response — the habits, avoidance, or reactions that often reinforce those same beliefs.
Rather than digging endlessly into your past, CBT keeps its focus on the present. It asks, “What’s happening right now that keeps you stuck?” And then it helps you test new ways of responding.
The Core Principles of CBT
At the core of CBT is the idea that your thoughts, feelings, and behaviors are interconnected. When one shifts, the others can too. For example, if you often think, “I always mess things up,” you might feel defeated before trying something new, which leads to avoidance, and the lack of new experiences reinforces the same belief.
CBT interrupts this loop by making the invisible visible. Once you start noticing those habitual thoughts, you can question them. Once you act differently, you collect new evidence about what’s possible. Over time, those small shifts begin to rewire how you relate to yourself and the world.
CBT also works best when it’s active. You don’t just talk about problems; you practice new skills between sessions. The work might feel uncomfortable at times, but that discomfort often signals growth.
Conditions Addressed by CBT
CBT was initially developed to treat depression, but its practical, skill-based nature means it’s now used for a wide range of issues. Therapists often use CBT for anxiety disorders, panic, phobias, post-traumatic stress (PTSD), obsessive-compulsive disorder (OCD), and insomnia. It can also help with eating disorders, substance use, chronic pain, and stress-related conditions.
Many people seek CBT not because of a diagnosis but because they want to stop feeling trapped in specific patterns — procrastination, overthinking, or people-pleasing, for example.
CBT can be used on its own or alongside medication, mindfulness practices, or other therapeutic approaches. Its flexibility makes it suitable for both short-term relief and long-term growth.
Typical CBT Session Structure
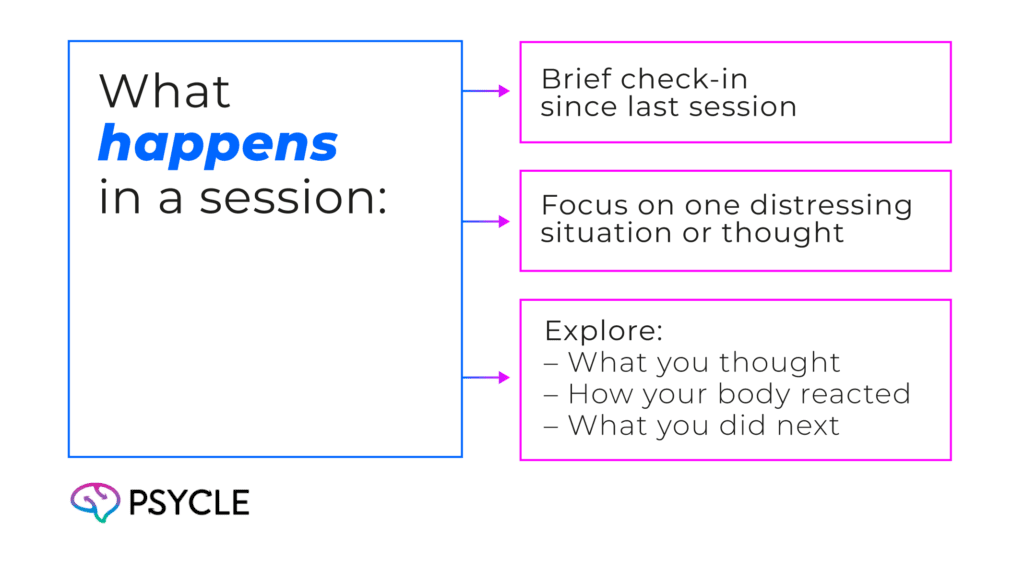
CBT sessions are usually structured and time-limited. You and your therapist agree on specific goals and meet regularly, often on a weekly basis, over a set number of sessions, typically between six and twenty.
A typical session might begin by reviewing what has happened since the last meeting, then focusing on a particular thought pattern or situation that has caused distress. Together, you explore what went through your mind, how your body reacted, and what you did next. You then identify alternative ways of thinking and behaving that could bring different results.
Therapists often assign between-session exercises, not in the traditional sense of homework, but as opportunities to practice newly acquired skills in daily life. This might involve noticing automatic thoughts, experimenting with a feared situation, or recording emotional reactions in a journal.
CBT is collaborative. You and your therapist work as partners. The therapist guides, but you bring the insight and effort that make change possible.
Examples of CBT Techniques
Several core techniques shape the practical side of CBT. One of the most common techniques is cognitive restructuring, which involves identifying distorted thoughts and replacing them with more balanced alternatives. Instead of assuming, “I failed once, so I’ll always fail,” you learn to challenge that belief with evidence and nuance.
Another standard method is behavioral activation, which helps lift a low mood by gradually re-engaging in meaningful activity. Rather than waiting to feel motivated, you act first, and the mood often follows.
Exposure techniques help with anxiety and trauma by teaching the nervous system that feared situations can be faced safely. These are handled gently and intentionally, always at a pace you can manage.
CBT also utilizes tools such as journaling, thought records, and relaxation strategies to track progress and solidify new habits.
Evidence & Effectiveness of CBT
CBT is one of the most scientifically tested forms of therapy. Decades of research across cultures, ages, and conditions consistently show that CBT reduces symptoms of depression and anxiety, helps prevent relapse, and improves quality of life.
Because it’s structured and easy to measure, CBT is often used to compare the effectiveness of other types of therapy. Organizations like the American Psychological Association recommend CBT as a first-line treatment for many mental-health concerns.
That said, CBT isn’t magic. Some people require a more comprehensive or relational approach to healing. It may not reach deep trauma on its own, mainly when the roots of distress lie in early attachment wounds. But even then, CBT’s tools can offer stability and clarity as part of a broader journey.
Who is Cognitive Behavioral Therapy Right For?
CBT suits people who are motivated to take an active role in therapy. If you like structure, clear goals, and practical exercises, you may find CBT especially effective.
It can also help if you feel lost in your emotions or want to develop tools for self-management. CBT therapy doesn’t demand that you have everything figured out, only that you’re willing to explore and practice.
When choosing a therapist, look for someone trained in CBT techniques and accredited by a recognized body. The therapeutic relationship still matters deeply: you need to feel safe, understood, and supported. CBT can be conducted in individual, group, or online formats, and many people find digital options to be surprisingly effective.
CBT and Psychedelic-Assisted Therapy
Though it’s a long-established approach, CBT continues to find new applications. It is increasingly used as an additional processing tool to support people in getting the best out of therapeutic experiences with psychedelics. CBT provides a structured framework for preparation, navigating the experience itself, and building its lessons into your life afterward.
When you enter the shifting landscape of a psychedelic-assisted session, you may feel parts of your mind loosen, perceptions open, and old patterns soften. In that space and the weeks and months that follow, Cognitive Behavioral Therapy can serve as a guiding compass.
Therapists working with psychedelic and ketamine-assisted approaches often find that CBT helps anchor the insights that emerge, turning fleeting breakthroughs into steady shifts in how you think, feel, and move through the world.
FAQs
How Long Does CBT Usually Last?
CBT is often a short-term treatment, typically consisting of between six and twenty sessions, although the exact length depends on your goals and the complexity of the issues you’re addressing. Some people choose to continue periodically to maintain progress.
Can CBT Work for Everyone?
Many people benefit from CBT, but it requires active participation. It may not fit everyone, especially if your struggles feel less about thought patterns and more about deep emotional or relational wounds. In such cases, CBT can still offer helpful tools in conjunction with other therapies.
What Makes CBT Different from Other Therapies?
CBT focuses on what’s happening right now; your thoughts, emotions, and actions in the present moment; and uses structured exercises to change them. It’s collaborative, time-bound, and measurable, making it especially useful for those who want clear strategies for everyday life.
Sources
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9667129/
- https://www.ncbi.nlm.nih.gov/books/NBK470241/
- https://www.youtube.com/watch?v=PsDzxBPET2I
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2851097/
- https://cogbtherapy.com/cbt-model-of-emotions
- https://www.youtube.com/watch?v=Yw1p9YlZKEU
- https://solportal.ibe-unesco.org/articles/neuroplasticity-how-the-brain-changes-with-learning/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7613897/
- https://journals.sagepub.com/doi/10.1177/1755738012471029
- https://medicine.umich.edu/sites/default/files/content/downloads/Behavioral-Activation-for-Depression.pdf
- https://www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/position-statements/pharmacologically-assisted-psychotherapy-research-guidance.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9850872/

