Post-Traumatic Stress Disorder (PTSD) and Complex Post-Traumatic Stress Disorder (CPTSD) both result from exposure to trauma, but they differ in causes, symptoms, and treatment approaches. This article delves into the causes and symptoms of PTSD and CPTSD, offering key insights into their complexities and avenues for support.
Key Takeaways
- PTSD is generally triggered by a single traumatic event, whereas CPTSD stems from prolonged or repeated trauma.
- Both conditions share symptoms like hypervigilance, intrusive memories, and emotional numbness, but CPTSD impacts emotional regulation and relationships more significantly.
- Treatment for PTSD includes therapies like TF-CBT and EMDR, while CPTSD requires a more multifaceted approach, incorporating additional therapies like DBT and somatic therapies.
- Emerging treatments, such as ketamine therapy, show promise in alleviating symptoms of both PTSD and CPTSD.
What is PTSD?
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that develops after experiencing or witnessing a traumatic event, such as an accident or assault. The condition emerges when the brain and body’s natural stress response fails to reset from these initial triggers, leading to hypervigilance, a chronic state of heightened alertness.
These incidences can also cause emotional numbness as the brain tries to protect itself from emotional pain related to the trauma. PTSD is also characterized by intrusive memories and flashbacks related to the event. These core symptoms can interfere with sleep, relationships, and other aspects of daily life.
Understanding Complex Trauma
Complex Post-Traumatic Stress Disorder (CPTSD) goes beyond PTSD by adding layers of complexity stemming from specific types of trauma. It often arises from prolonged or repeated traumatic experiences, such as chronic abuse, that tend to occur in early life.
CPTSD shares core symptoms with PTSD but has an additional impact on self-concept, emotional regulation, and interpersonal relationships. The “complex” aspect reflects the cumulative effects of long-term trauma on an individual’s emotional and psychological well-being.
Common Causes of PTSD vs. CPTSD
PTSD is frequently linked to singular, acute traumatic events that occur abruptly and create an immediate sense of threat. On the other hand, CPTSD develops from enduring trauma, often in situations where the victim feels trapped.
Examples of PTSD Causes
- Combat exposure: Military personnel experiencing or witnessing life-threatening combat situations.
- Sexual assault: Victims of rape or sexual violence.
- Childhood abuse: Physical, emotional, or sexual abuse during childhood.
- Natural disasters: Experiencing events such as hurricanes, earthquakes, or floods.
- Accidents: Being involved in a serious car crash, industrial accident, or plane crash.
- Terrorist attacks: Witnessing or being a victim of terrorist activity.
- Death of a loved one: Sudden loss or witnessing the violent death of a close family member or friend.
- Physical assault: Victims of violent crime such as robbery or assault.
- Witnessing violence: Observing the violent injury or death of others.
Examples of Causes of CPTSD
- Chronic childhood abuse: Long-term physical, emotional, or sexual abuse in childhood.
- Neglect: Ongoing emotional or physical neglect during formative years.
- Long-term domestic violence: Extended exposure to intimate partner violence or abusive relationships.
- Living in war zones: Extended exposure to conflict, war, or displacement.
- Human trafficking: Being a victim of human trafficking and exploitation over an extended period.
- Cult or extreme group involvement: Being part of a cult or experiencing severe manipulation or exploitation by a group.
- Repeated sexual assault: Ongoing sexual violence over an extended period.
- Chronic bullying: Prolonged and severe bullying during childhood or adolescence.
- Ongoing emotional or psychological manipulation: Experiencing long-term psychological or emotional abuse.
Neurological Differences Between PTSD and CPTSD
Research indicates that PTSD and CPTSD have distinct neurological patterns. Both conditions involve alterations in brain regions responsible for processing fear, emotions, and memory, but the extent and specific changes differ.
Studies using functional MRI (fMRI) have found that individuals with PTSD often exhibit heightened activity in the amygdala—the brain’s fear center—and reduced activity in the prefrontal cortex, which regulates emotional responses.
Similar changes occur in CPTSD, but they may be more severe. Additional brain areas related to self-perception and emotional regulation are affected, such as the anterior cingulate cortex and orbitofrontal cortex.
Diagnosis Challenges
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is the handbook used by healthcare professionals in the United States and much of the world as a guide to diagnosing mental health disorders. The DSM-5 currently doesn’t recognize CPSD as its own condition but rather includes symptoms within its definition of PTSD.
Because CPTSD is not officially recognized in the DSM-5, it is often underdiagnosed or misdiagnosed with other mental health disorders, such as borderline personality disorder, depression, or generalized anxiety disorder.
However, the International Classification of Diseases 11 (ICD-11), another diagnostic handbook created by the World Health Organization, has a defined diagnosis for CPTSD. Clinicans worldwide are increasingly recognizing the disorder, making it easier for people to get a diagnosis.
Treatment Approaches
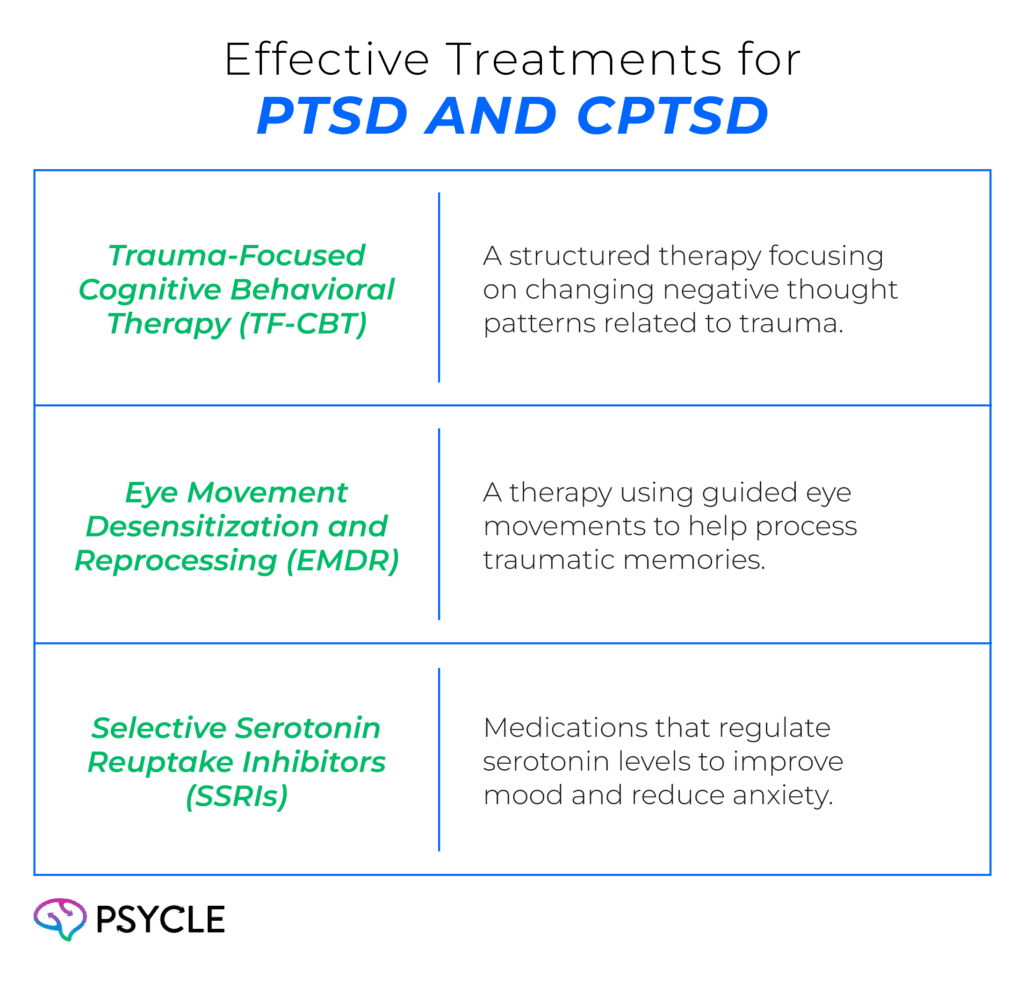
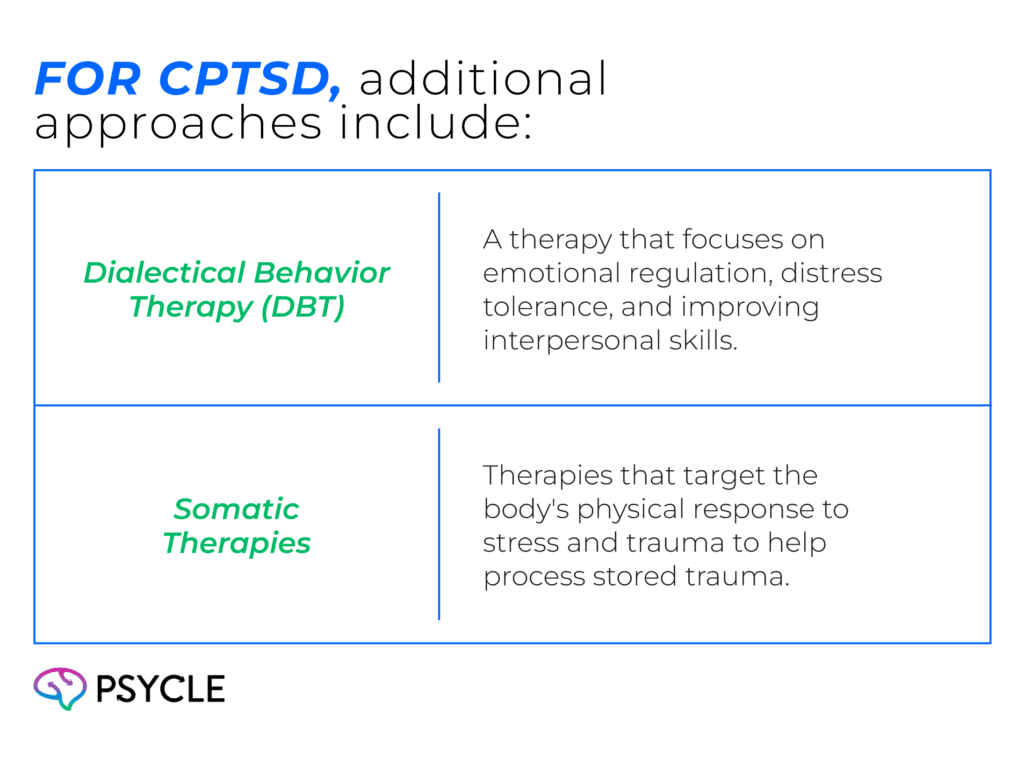
CPTSD treatment is typically longer and more multifaceted to address the broader symptoms. Emerging treatments, such as ketamine therapy, show promise in improving mood regulation and promoting neuroplasticity to alleviate both PTSD and CPTSD symptoms.
Seeking Help
For those grappling with PTSD or CPTSD, numerous resources are available to support recovery. National organizations, local support groups, and trauma-informed therapists offer specialized care for PTSD and CPTSD.
Professional help is crucial in navigating the complexities of these conditions, offering a pathway to relief, resilience, and improved quality of life. If you or a loved one is struggling, reaching out to a mental health professional is a vital step toward recovery.
Frequently Asked Questions
How Do PTSD and CPTSD Differ in Their Causes?
PTSD is typically caused by a single traumatic event, such as a car accident or assault. In contrast, CPTSD develops from prolonged exposure to trauma, often from chronic abuse, neglect, or living in an abusive or war-torn environment.
Why is CPTSD Harder to Diagnose than PTSD?
CPTSD is not officially recognized as a separate condition in the DSM-5, leading to misdiagnosis or underdiagnosis. It is often confused with other mental health conditions, such as borderline personality disorder or depression. However, the ICD-11 recognizes CPTSD, making it easier for clinicians worldwide to diagnose.
Can Medications Alone Help with PTSD or CPTSD?
Medications like SSRIs can help alleviate symptoms of PTSD and CPTSD, particularly in managing anxiety and depression. However, therapy is often necessary for effective treatment, as it addresses the root causes and emotional difficulties associated with these disorders.