Schizophrenia is a mental disorder marked by hallucinations, delusions, and disorganized thinking. With classical psychedelics producing similar effects, there is concern that these drugs can cause schizophrenia. However, the relationship is more complicated.
This article explores the research into psychedelics and schizophrenia, discussing the risks, overlap, neurobiology, and the potential for these drugs to even help treat symptoms.
Key Takeaways
- Early scientists thought psychedelics could mimic schizophrenia, but these narratives have since changed.
- Psychedelics can trigger psychosis in people at high risk, but it’s unlikely they cause schizophrenia in most users.
- Brain scans show similar patterns between psychedelic states and schizophrenia, but the experiences are different.
- Psychedelics may be trialled to help treat schizophrenia someday, but research is still in early stages.
Early Research: Psychedelics as Psychomimetics
The first wave of psychedelic research began after LSD was discovered in 1943. At first, scientists were interested in how psychedelics could help them understand schizophrenia and other psychotic disorders. They called these substances psychomimetics, meaning they mimic psychosis, because they cause hallucinations and distorted thinking.
However, researchers realized that the psychedelic state was not the same as psychosis and began to see that these drugs might have therapeutic benefits. This shifted the focus of research.
Instead of only studying how psychedelics relate to psychosis, scientists started exploring how they could be used to aid psychotherapy and improve mental health. Most studies focused on using psychedelics in therapy to treat addiction, but they were also tested for neurosis (which includes symptoms of anxiety and depression) and schizophrenia.
The War on Drugs and Its Impact
In the 1970s, the U.S. government began the War on Drugs, led by President Nixon. Psychedelics were classified as Schedule I substances under the Controlled Substances Act of 1970. This brought the first wave of psychedelic research to a halt.
During this time, the media played a major role in shaping public opinion. News stories and tabloid headlines warned that psychedelics, especially LSD, could cause schizophrenia. This idea became deeply rooted in public belief.
Although there is some connection between psychedelics and psychosis, newer research is offering a different perspective. A second wave of psychedelic studies is now focusing on their potential therapeutic benefits and shifting the conversation once again.
Can Psychedelics Cause Schizophrenia?
There have been many case reports of psychedelics triggering psychotic episodes that resemble schizophrenia. Both involve hallucinations, delusions (false beliefs), disorganized thinking, and a loss of contact with reality.
Most of the time, they are short and go away in a few hours or days, but there have been cases of them lasting longer.
A 2024 study from Canada found that people who went to the emergency room after using psychedelics were 21 times more likely to later be diagnosed with schizophrenia compared to the general population.
However, when the researchers accounted for whether these individuals already had a mental health or substance use disorder, the risk dropped to 3.5 times more likely. It’s important to note that the study only looked at people who were hospitalized due to psychedelic use, so the findings don’t apply to all users.
Larger studies that consider general psychedelic use tell a different story. In 2015, a Norwegian study found no heightened risk of mental health problems, including psychosis, among individuals who used classical psychedelics. The data was based on responses from over 135,000 U.S. drug survey participants.
Experts believe the risk is higher in people who already have risk factors. These include:
- A personal or family history of psychosis
- Trauma or high stress
- Other mental health disorders
The Neuroscience of Psychedelics & Schizophrenia
Both psychedelics and schizophrenia change how the brain works. Some of these changes are similar.
One example is hyperfrontality, which is increased activity in the prefrontal cortex (PFC). This brain area is responsible for decision-making, attention, self-awareness, and filtering incoming information.
When this area becomes overly active, it can disrupt normal brain function and lead to distorted thinking and sensory processing. Hyperfrontality is seen during psychedelic experiences and in early schizophrenia.
However, in long-term schizophrenia, brain scans often show hypofrontality, which is reduced activity in the PFC over time.
Another key similarity is increased brain entropy. In neuroscience, entropy refers to the level of randomness or unpredictability in brain activity. In both psychedelic states and schizophrenia, brain networks become more flexible and less constrained by normal patterns.
This rise in entropy explains unusual thinking, confusion, and a loss of a clear sense of reality.
Are Psychedelic Trips Like Schizophrenic Episodes?
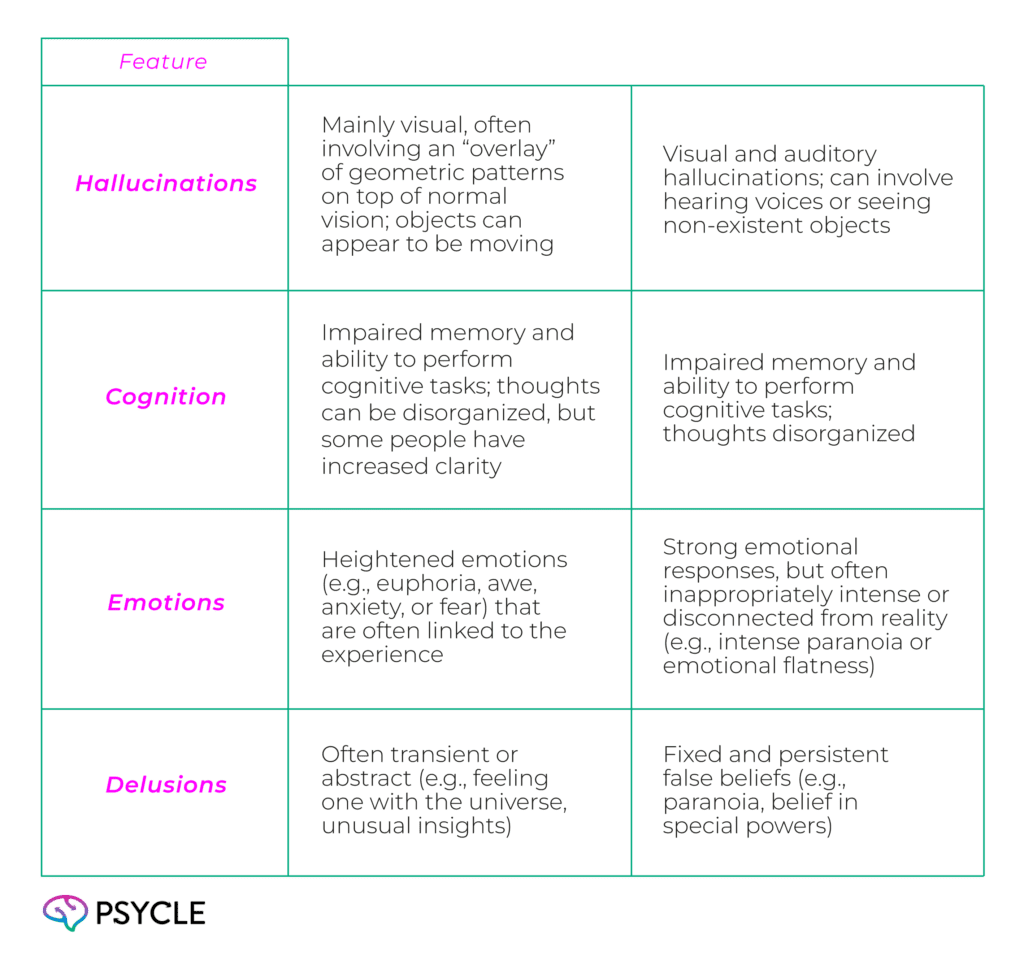
While psychedelics and schizophrenic episodes share similarities, there are also some key differences.
In preliminary research from the University of Alabama, people who had experience with both psychosis and psychedelic experiences said they were not the same. They said they felt more clarity and more control when using psychedelics compared to a psychotic episode.
Some reported that cannabis was more similar to an episode than classical psychedelics.
Similarities and Differences Between Psychedelics and Schizophrenia
Can Psychedelics Treat Schizophrenia?
Psychedelic-assisted therapy to treat schizophrenia and other psychotic disorders is an emerging area of research. While no formal studies have been conducted yet, researchers believe that psychedelic-assisted therapy could help patients with schizophrenia, especially in addressing negative symptoms like flattened emotion and anhedonia (the inability to feel pleasure).
Several studies have shown that psychedelics can have long-lasting positive effects in treating depression, which has many crossovers with negative symptoms of schizophrenia. Additionally, psychedelics have been shown to promote neurogenesis, the growth of new nerve cells, which could help repair brain tissue lost in areas affected by schizophrenia.
However, this area of research is still in its early stages. Due to the unknown risks, patients with a personal or family history of psychotic disorders are currently excluded from psychedelic clinical trials.
Moreover, while psychedelics could have benefits for schizophrenic patients, this would be under the highly regulated, supervised context of psychedelic-assisted therapy.
Final Thoughts
The link between psychedelics and schizophrenia is still not fully understood. While there are similarities between the two, there are also crucial differences. Psychedelics are unlikely to cause schizophrenia in people without a predisposition. However, they could trigger a psychotic episode or lead to chronic schizophrenia in those who are already at risk.
If you have a personal or family history of schizophrenia or other risk factors, we recommend that you avoid using psychedelics.
FAQs
Are Psychedelics Safe for Bipolar Disorder With Mania?
Again, this relationship is complex. There have been case reports of mania-onset following psychedelic use in people with bipolar disorder. However, research has also shown psilocybin therapy can be safe and beneficial for people with bipolar disorder when used in a controlled, supported setting.
Are Some People With Schizophrenia More Sensitive to Psychedelics than Others?
Yes, individuals with schizophrenia can vary in their sensitivity to psychedelics. Those with more severe symptoms or co-occurring disorders may experience stronger adverse reactions.

