With the rise of treatment-resistant depression (TRD) and the approval of esketamine as a novel antidepressant, understanding its potential for addiction and the implications of its use is crucial.
This article explores the prevalence of TRD, the benefits and risks of esketamine, and the challenges in monitoring its use.
Key Takeaways
- Esketamine is approved for treating treatment-resistant depression (TRD) and is administered as a nasal spray.
- It provides rapid relief from depressive symptoms, acting within hours compared to weeks for traditional antidepressants.
- Short-term risks include dissociation, hallucinations, and cognitive impairment; long-term risks may involve bladder damage and cognitive decline.
- Psychological dependence is a significant concern due to esketamine’s psychoactive properties.
- Telehealth use of esketamine requires stringent monitoring to prevent misuse and ensure patient safety.
Prevalence and Burden of Treatment-Resistant Depression
Major depressive disorder (MDD) affects millions of people across the globe, and its prevalence is continuing to rise. Depression is typically treated with a combination of talk therapy and antidepressants, the most common being selective serotonin reuptake inhibitors (SSRIs).
This includes fluoxetine (Prozac), citalopram (Cipramil) and escitalopram (Cipralex).
Though effective for some, an estimated 30-40% of those with depression are treatment-resistant. The Institute for Clinical and Economic Review defines treatment-resistant depression (TRD) as “patients with persistent depression after attempted management with two or more medications.”
TRD causes suffering to those affected and their loved ones and is also a major source of economic burden. In 2019, the cost of MDD was estimated to be $333.7 billion, equating to around $16,854 per adult.
Esketamine: A Novel Antidepressant Therapy
Ketamine, traditionally used as an anesthetic, emerged as a groundbreaking antidepressant over the past ten years. In 2000, Yale School of Medicine researchers published the first randomized controlled trial highlighting ketamine’s antidepressant effects.
Multiple studies have echoed these findings and, importantly, demonstrated that ketamine can decrease symptoms in people with TRD.
Unlike SSRIs and other conventional antidepressants, ketamine has a strong interaction with NMDA receptors in the brain. This unique mechanism of action is thought to contribute to its rapid-onset and long-lasting antidepressant effects.
This interaction with NMDA receptors also induces a dissociative effect, which can be pleasurable for some. As NMDA receptors are involved in neuroplasticity, the basis of learning and behavior, this interaction also increases the risk of learned addictive behaviors (more about esketamine addiction below).
Ketamine is a racemic mixture, meaning that it contains two mirror-image molecules called enantiomers. Esketamine is one of these enantiomers and was approved for TRD by the FDA in 2019. Esketamine has a higher potency than ketamine and can be administered intranasally, unlike ketamine, which is provided through injection.
As with ketamine, clinical research shows esketamine has antidepressant effects in treatment-resistant patients. However, the evidence regarding its long-term efficacy is mixed.
Esketamine and Suicidal Ideation
As well as mood symptoms, esketamine can also help reduce suicidal ideation in depressed patients. Pooled data from two esketamine trials found that all 465 patients included had reduced severity of suicidality 24 hours after treatment.
Pharmacokinetics and Administration
Esketamine is primarily administered as a nasal spray, allowing rapid absorption through the nasal mucosa directly into the bloodstream. This administration route bypasses the liver, leading to a quicker onset of action compared with orally administered drugs.
Esketamine stays in the bloodstream for around seven to twelve hours before it is broken in the liver, and its metabolites are excreted through urine.
Clinically, esketamine is administered under medical supervision to monitor for any adverse effects, given its potential for dissociation and other potentially harmful side effects (see more below).
The initial dosing usually involves twice-weekly administration for the first four weeks, followed by a maintenance phase with doses tapered to weekly or biweekly based on patient response and tolerability.
Is Spravato Addictive?
Spravato isn’t typically considered physically addictive in the way opioids or some other drugs are. However, chronic use has been known to cause psychological dependence, a compulsion or perceived need to continue using a substance to experience its psychological effects.
Unlike physical dependence, which involves physiological withdrawal symptoms, psychological dependence manifests through cravings, emotional distress, and mental preoccupation with the substance, often leading to habitual use.
This risk of psychological addiction is partly due to ketamine’s psychoactive and dissociative properties., which can be pleasurable and euphoric for some. People with deep-rooted trauma may also find psychological relief from their negative thoughts when using esketamine and compulsively use the drug to escape.
The risk of addiction is particularly concerning in the context of telehealth, where patients are provided ketamine to take at home without the direct supervision of patients.
In an investigation for The New York Times, several instances of telehealth patients abusing ketamine were identified. Journalist Chris Hamby commented, “Chasing the lost high, they sought increased doses, took multiple days’ worth at once, or altered the medicine to release more of its payload.”
Efficacy and Safety of Esketamine
Short-term risks of esketamine tend to disappear once the drug has worn off, but may last up to 24 hours. These include:
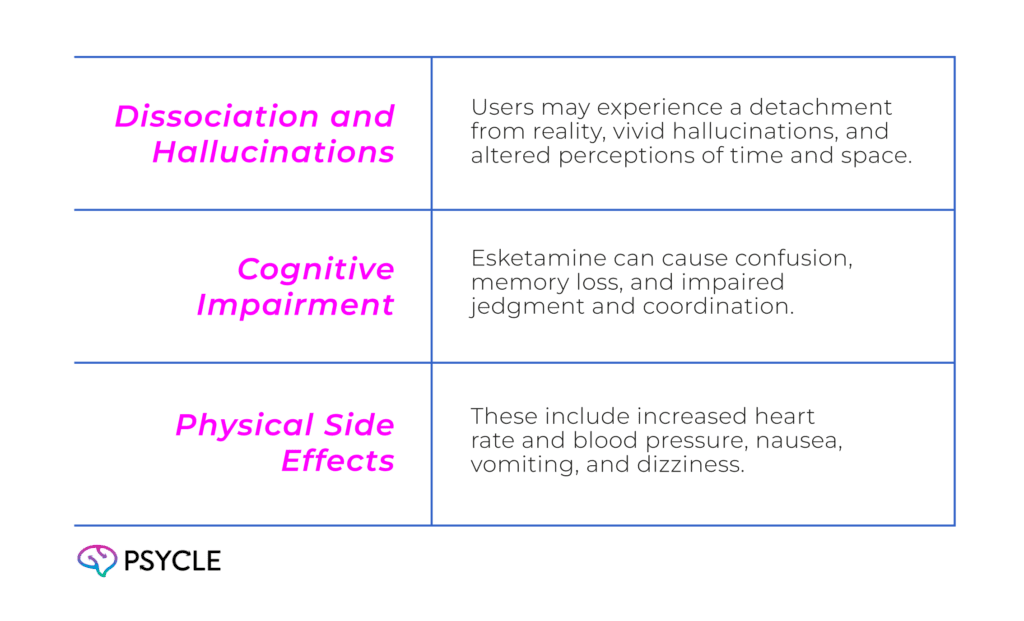
As mentioned, esketamine use may lead to addiction, characterized by cravings and withdrawal symptoms upon cessation. Chronic long-term use can cause bladder and urinary tract damage, which may lead to severe pain and incontinence. Abuse has also been associated with cognitive impairment and kidney and liver damage.
Risk Factors and Monitoring
Identifying Potential Risks
Because of esketamine’s addictive potential, those with a substance abuse disorder are not permitted to receive esketamine, according to the drug’s criteria for use. Those with cardiovascular-related problems, pregnancy, seizures and psychotic disorders are also included on the exclusion list.
Monitoring and Management
Patients receiving esketamine should undergo thorough initial assessments and regular follow-ups to monitor response, side effects, and adherence to their prescription regimen.
In-person administration in a controlled clinical setting is often preferred to mitigate risks. However, protocols such as virtual check-ins and remote monitoring technologies are in place in telehealth.
Regulatory Oversight and Guidelines
The Food and Drug Administration (FDA) approved esketamine as SPRAVATO in 2019. According to their guidelines, SPRAVATO is to be administered under the supervision of a healthcare professional (which may be virtually in the case of telehealth).
A patient’s blood pressure should be measured before and after administration. Evidence of therapeutic benefit should be evaluated at the end of the induction phase to determine the need for continued treatment.
The detailed guidelines can be accessed here: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/211243lbl.pdf
FAQs
How is Esketamine Monitored and Managed, Especially with Telehealth?
Patients require thorough assessments and regular follow-ups to monitor response and side effects. Telehealth protocols include virtual check-ins and remote monitoring to ensure safe usage and prevent misuse.
What are the Short-Term and Long-Term Risks of Esketamine Use?
Short-term risks include dissociation, hallucinations, and cognitive impairment, while long-term use can lead to bladder damage, cognitive decline, and potential psychological dependence.
How Does Esketamine Help with Treatment-Resistant Depression?
Esketamine acts on NMDA receptors in the brain, leading to rapid and sustained antidepressant effects, which is particularly beneficial for those who do not respond to traditional treatments.

