Dreams are a fascinating and often mysterious part of our sleep experience, deeply tied to our mental and emotional well-being. When taking antidepressants, many people notice changes in their dreaming—some subtle, others more pronounced.
This article explores how different classes of antidepressants affect dreaming, why these drugs affect dreaming and what those changes might mean for mental health.
Key Takeaways
- Antidepressants often alter REM sleep—either reducing its duration or changing its quality—which can lead to vivid, emotionally intense dreams that may be beneficial for emotional processing or, conversely, cause nightmares and disrupted sleep.
- Different classes of antidepressants affect dreaming in distinct ways: SSRIs and SNRIs commonly reduce REM but increase dream vividness, while older drugs like MAOIs and TCAs tend to suppress REM or alter dream recall depending on the medication.
- Changes in serotonin levels, which influence both melatonin production and REM sleep, help explain why antidepressants impact dreaming, and REM rebound may account for the vividness that follows REM suppression.
How Depression Affects Dreaming: Changes in REM Sleep and Dream Content
There is a well-established link between depression and sleep. In general, sleep disorders are more common in people with depression. But while some people experience insomnia, characterized by an inability to stay and fall asleep, others experience hypersomnia, characterized by excessive sleepiness despite adequate sleep.
The disruption of regular sleep in depression can have a significant impact on dreaming. In particular, depression disrupts REM (rapid eye movement) sleep, which is the stage in people’s sleep where vivid dreams occur.
People with depression tend to have reduced dream recall compared to non-depressed individuals, meaning they remember fewer dreams upon waking. Yet, when dreams are remembered, they tend to have a more negative emotional tone, often featuring sadness, fear, or feelings of hopelessness.
Because depression and sleep are closely connected, researchers have long been interested in how antidepressants affect sleep architecture—the structure and stages of sleep throughout the night. Many antidepressants change the timing, length, and quality of REM sleep, which can in turn alter dreaming.
Scientists are still exploring whether these changes are helpful or if they are side effects that need to be managed.
How Different Antidepressants Affect Sleep and Dreams
Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective Serotonin Reuptake Inhibitors (SSRIs) are the most widely used antidepressants. They’re a first-line treatment, meaning they’re the most preferred medical option, along with talk therapies. These drugs work by increasing the availability of the neurotransmitter serotonin in the brain by blocking it from being reabsorbed. Serotonin is a chemical messenger that plays a crucial role in regulating mood and emotions.
In general, SSRIs are found to have adverse effects on sleep, increasing sleep interruption and reducing the amount of REM sleep. Interestingly, while SSRIs reduce REM, fluoxetine users commonly report more vivid dreams. Moreover, studies show escitalopram increases dream recall.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) are also a first-line depression treatment. They work similarly to SSRIs but inhibit the reabsorption of norepinephrine, as well as serotonin. Norepinephrine plays a key role in both mood and energy levels.
Studies show users of venlafaxine may have more vivid dreams, frequent nightmares, and symptoms of REM Behavior Disorder (RBD), where individuals physically act out their dreams during sleep. Duloxetine shows a similar effect, reducing REM sleep time while increasing sleep interruptions and limb movements during sleep.
Monoamine Oxidase Inhibitors (MAOIs)
Monoamine Oxidase Inhibitors (MAOIs) are older antidepressants that affect the monoamine neurotransmitters serotonin, dopamine, and norepinephrine. They’re relatively uncommon and only used today for treatment-resistant depression (TRD), when other first-line antidepressants haven’t worked.
One study found that phenelzine significantly suppressed REM sleep. Those who responded positively to the medication had reduced dream recall.
Tricyclic Antidepressants (TCAs)
Like MAOs, tricyclic antidepressants (TCAs) are only used in depression treatment when the first-line medications have failed to work. They’re also used in cases where people have both depression and anxiety, OCD, or panic disorders, since they have a calming effect. These drugs work by inhibiting monoamine reuptake channels for monoamines, but are less selective than SSRIs and SNRIs.
Because of their sedating effects, TCAs are often used to treat chronic insomnia in addition to depression. These medications are linked to improved sleep quality and longer sleep duration. Most research finds these drugs don’t affect dreaming. However, in one study, depressed patients who used Timipramine had less dream recall and more positive dream emotions after four weeks.
Antidepressants and Vivid Dreams: A Common Side Effect
One of the most commonly reported side effects of antidepressant use is an increase in vivid dreaming. People often describe their dreams as more intense, detailed, and emotionally charged. This effect is likely to occur because of how antidepressants affect REM sleep.
The Potential Benefits and Downsides of Vivid Dreams
In some cases, vivid dreams may be a positive sign that emotional processing is taking place. Since dreams are thought to help the brain work through emotions, stress, and unresolved experiences, vivid dreaming could indicate that antidepressants are facilitating deeper psychological healing.
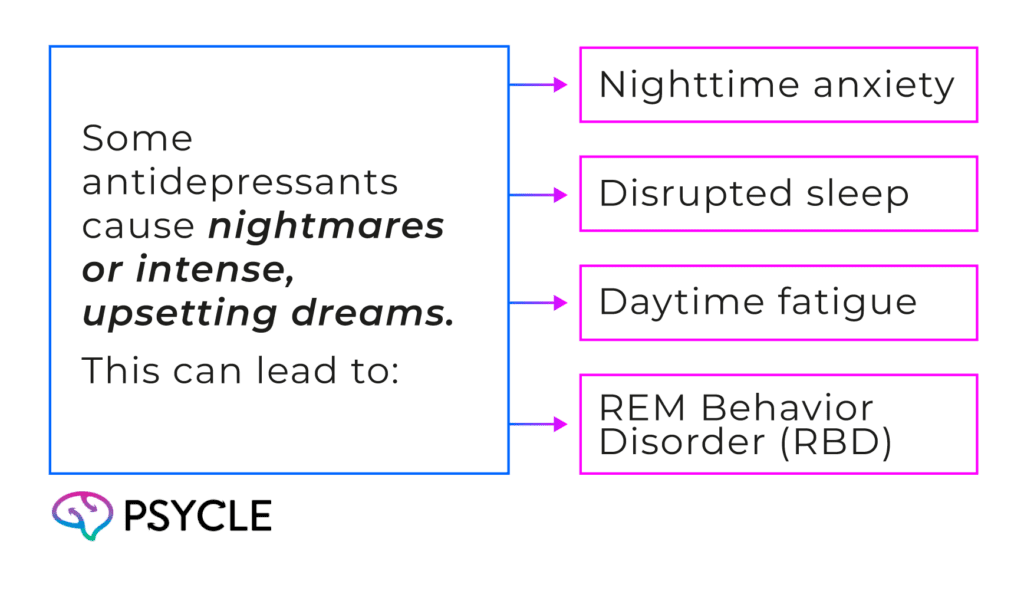
However, not all vivid dreams are pleasant. For some people, antidepressants trigger nightmares, disturbing imagery, or dreams that feel emotionally overwhelming. This can lead to:
The Science Behind How Antidepressants Affect Dreaming
The circadian rhythm is the body’s internal clock. It runs on a roughly 24-hour cycle and helps regulate essential functions, such as body temperature, hormone levels, and sleep. One of the main hormones involved in this rhythm is melatonin.
When it’s dark, the brain produces melatonin to help calm the body and signal that it’s time to sleep. When it’s light, melatonin production is suppressed, helping you stay awake and alert.
Since melatonin is made from serotonin, changes in serotonin levels caused by antidepressants can influence melatonin production and influence the sleep cycle. Research also shows that serotonin helps suppress REM sleep, the stage during which most dreaming occurs, which may explain why antidepressants reduce both the duration of REM sleep and dream recall.
It may seem contradictory that antidepressants are associated with more vivid dreams, despite inhibiting REM. However, this could be explained by REM rebound, where the brain temporarily increases REM activity, making dreams feel more intense and emotionally powerful after it has been suppressed for a period of time.
FAQs
I’ve Been Having Nightmares Since Beginning Antidepressants. What Should I Do?
Nightmares can be a side effect of some antidepressants, especially during the first few weeks of treatment. It’s important to discuss this with your doctor, as they may adjust your dosage or suggest switching medications. They can also recommend sleep hygiene techniques or therapy to help manage distressing dreams.
Is Dreaming Good for Mental Health?
Yes, dreaming—especially during REM sleep—is believed to play a role in processing emotions, consolidating memories, and supporting overall psychological balance. While the content of dreams can vary, regular dreaming is generally considered a healthy sign of natural sleep cycles. However, when dreams are chronically distressing, this can have a negative impact on everyday life.

