Obsessive-Compulsive Disorder (OCD) is characterized by persistent, unwanted thoughts (obsessions), and ritualistic behaviors performed to alleviate anxiety (compulsions). This article will examine how early-life adversities could cause and influence OCD symptoms and consider the therapeutic benefits of addressing childhood trauma in OCD treatment.
Key Takeaways
- Childhood trauma has been proposed to increase the risk of developing OCD later in life.
Studies have shown that individuals with OCD often report a history of childhood trauma. - The exact mechanisms by which childhood trauma may influence the development of OCD are not yet fully understood.
- Further research is needed to better understand the relationship between childhood trauma and OCD.
- Addressing childhood trauma is an important aspect of managing OCD symptoms.
Understanding the Different Types of Childhood Trauma
Trauma is the physical and emotional response to highly distressing situations. Childhood trauma occurs during someone’s formative years, before the age of 18, and can have significant emotional, physical, and psychological consequences on their later adult life, such as the development of OCD.
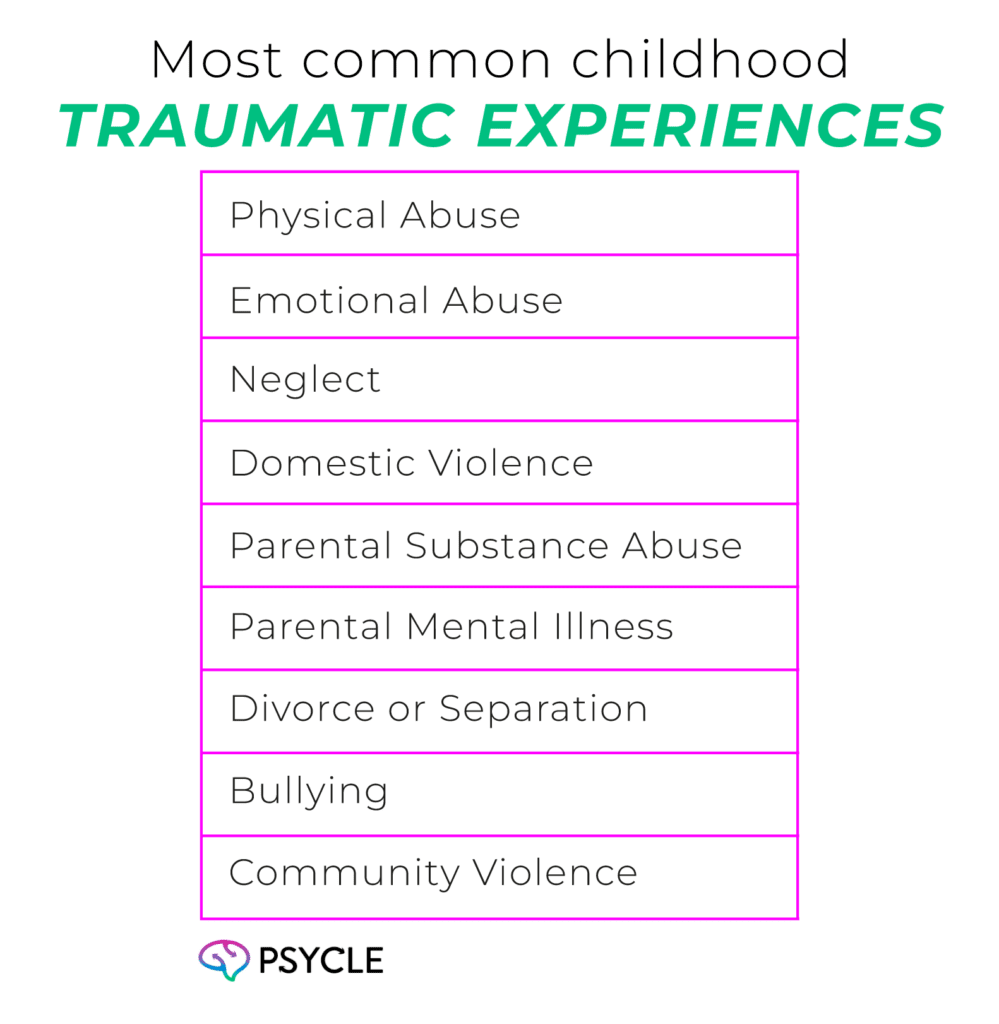
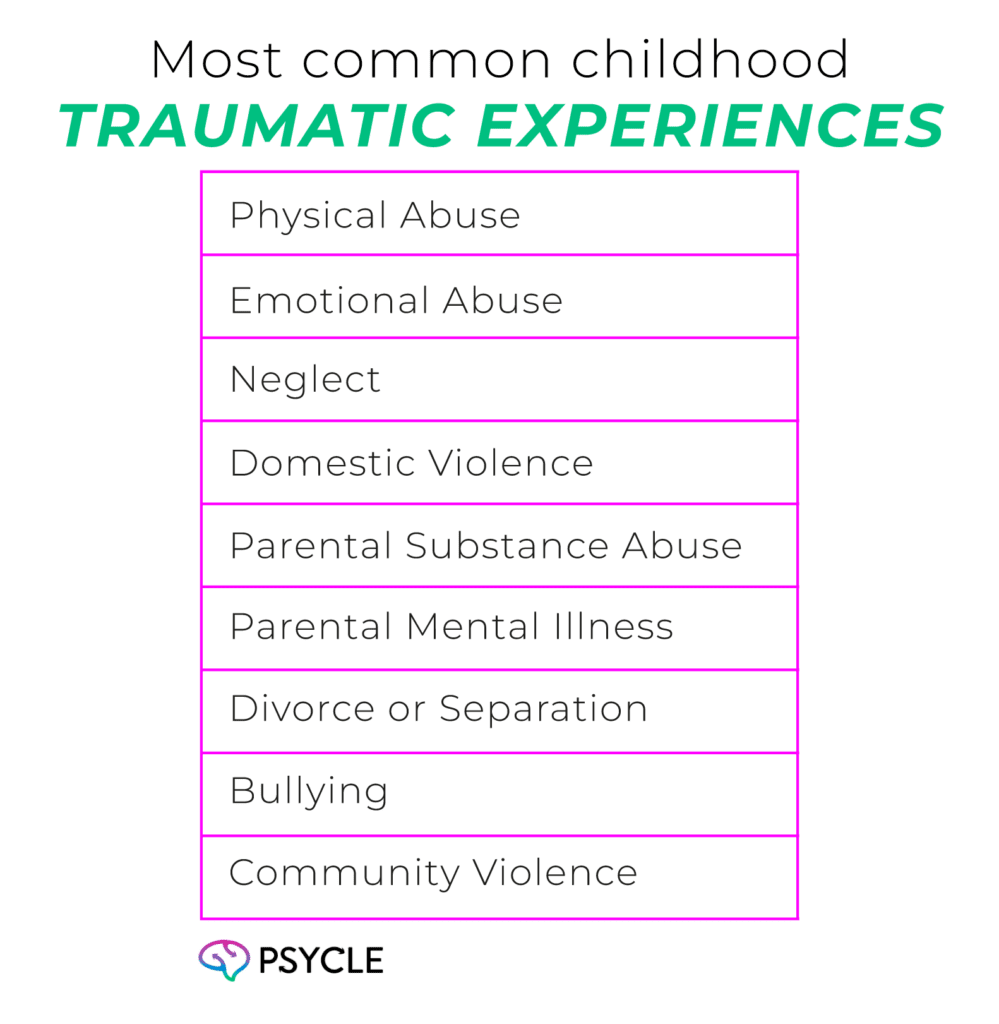
Childhood trauma is most associated with certain types of experiences. However, it can manifest as a result of any scenario in which a child is deeply disturbed.
The most common childhood traumatic experiences include:
Exploring the Prevalence of OCD and Childhood Trauma
Not all those with OCD have experience of childhood trauma. However, research shows a significant portion of OCD patients have experienced adverse events in younger life. A Chinese population study of 180 OCD outpatients found that 77% of patients reported at least one type of childhood trauma experience.
In an American study, only 13-30% of college students with diagnosable OCD met the criteria for childhood trauma, suggesting long-term mental health consequences are most likely to reveal themselves in adulthood. However, cultural factors could also explain the discrepancies between the two findings.
Can OCD Predict Symptom Severity?
OCD symptoms are generally divided into two categories: obsessions and compulsions. Obsessions include intrusive, unwanted, and distressing thoughts. Compulsions include repetitive behaviors and mental acts such as excessive washing and cleaning, counting and repeating certain words or phrases, and arranging or organizing items in a specific way.
Research shows childhood trauma may increase the severity of OCD symptoms. In a study of one hundred OCD outpatients, researchers showed greater childhood trauma experiences were associated with psychotic vulnerability, more severe symptoms, and an earlier age of OCD onset. The severity of impulses and rumination (repetitive thinking) were facets particularly associated with childhood trauma in another study.
The Science Behind Childhood Trauma and OCD: Potential Underlying Mechanisms
Genes, Stress, and OCD Onset
OCD may be influenced by genetic factors, given that the disorder typically runs through families and commonly occurs in twins, even if the twins are separated at birth. Genes involved in producing serotonin–a neurotransmitter involved in mood and behavior–are most associated with OCD.
The gene-environment interaction theory posits that genetic and environmental factors combine to trigger certain mental health outcomes. In the case of OCD, a combination of faulty serotonin genes and stressful life events, including childhood trauma, could be responsible for causing obsessive thoughts and behaviors.
OCD as a Maladaptive Coping Mechanism to Stress
Maladaptive coping mechanisms, which individuals often adopt to navigate the challenges posed by trauma, can become ingrained behavioral patterns. These coping mechanisms may involve attempts to regain a sense of control, avoid distressing thoughts or memories, or manage heightened feelings of responsibility.
Children exposed to trauma may develop rituals or compulsions as a way to cope with the overwhelming stress associated with the traumatic experiences. These behaviors can serve as a form of self-soothing or a means to prevent perceived harm or catastrophic events.
Over time, these maladaptive coping mechanisms can persist into adulthood.
How Childhood Trauma Rewires the Brain Toward OCD
During childhood, the brain is particularly malleable, and exposure to traumatic events can greatly influence the shaping of neural circuits. Childhood trauma may alter neural pathways involved in emotional processing, self-regulation, and habits, leading to the onset of OCD.
Brain studies show the cortico-striatal-thalamo-cortical (CSTC), a brain circuit that controls habit formation and reward, may be disrupted in OCD patients. Alterations in this neural circuit could be impacted by traumatic events in childhood.
Potential Factors Influencing the Relationship Between Childhood Trauma and OCD
Types and Severity of Trauma
The type and degree of traumatic experience a child has could determine how their symptoms manifest. For instance, sexual abuse may increase the likelihood of developing obsessions related to sexual or aggressive thoughts. Neglect could impact the development of OCD symptoms related to uncertainty and fear of abandonment.
One study found a positive association between the severity of childhood maltreatment and OCD symptom severity in 68 patients. Emotional abuse, sexual abuse, and neglect were the most common forms of trauma in their sample.
The Age at Which Trauma Occurred
Some evidence shows experiencing trauma at a younger age may increase the likelihood of developing mental health illnesses later in life. This could be because the brain is more plastic at a younger age, and it’s during these earlier stages in life that views about the world and how to behave are formed.
Exploring the Comorbidity of Childhood Trauma and OCD
Comorbidities–having multiple mental health illnesses–are common in OCD patients. In one study, 69% of over 15000 OCD individuals had comorbidities. The most common of which were mood disorders (mainly major depressive disorder), anxiety (generalized anxiety disorder and neurodevelopmental disorders (attention-deficit disorder).
Since childhood trauma is a risk factor for many mental health issues, having traumatic experiences during childhood may increase the chance of these comorbidities.
Addressing Childhood Trauma to Manage OCD Symptoms
Engaging in psychotherapy, mainly through approaches like Cognitive-Behavioral Therapy (CBT), can help individuals confront and overcome symptoms of Obsessive-Compulsive Disorder (OCD).
Psychotherapy offers a safe space for individuals to explore their symptoms and how they may relate to earlier life events. Empathy and compassion towards oneself can be cultivated by gaining insights into the developmental roots of one’s disorder. A therapist can also support someone to develop new, healthier thoughts and behaviour patterns, and coping mechanisms to stressful events.
Conclusion
Childhood trauma may shape neural circuits and trigger maladaptive coping mechanisms, contributing to the development of Obsessive-Compulsive Disorder (OCD), as well as other psychological illnesses. The type and severity of trauma may further influence the relationship between childhood trauma and OCD.
Psychotherapy, especially Cognitive-Behavioral Therapy (CBT), provides a crucial avenue for individuals to confront and overcome OCD symptoms rooted in early experiences.
FAQs
Where Can I Find Further Reading on the Link Between Childhood Trauma and OCD?
For those interested in delving deeper into the complex relationship between childhood trauma and OCD, there is a wealth of further reading available. Numerous studies have explored the association between childhood trauma and OCD symptoms, with varying results. Additionally, expert opinions and reviews provide valuable insights into the topic. By exploring this literature, readers can gain a comprehensive understanding of the current research and expert perspectives on the link between childhood trauma and OCD.
What is the Prevalence of OCD and Childhood Trauma?
OCD is a relatively common mental disorder, with a lifetime prevalence rate of 1-2%. In comparison, the prevalence of childhood trauma, which includes various types of abuse and neglect, is estimated to be much higher. Understanding the prevalence rates of OCD and childhood trauma can help shed light on the scope of this issue and its potential impact on mental health.
Can Childhood Trauma Predict OCD Severity?
Studies have examined the relationship between childhood trauma and OCD severity, with mixed findings. Some research suggests that individuals with OCD who have experienced childhood trauma may exhibit more severe obsessions and compulsions compared to those without a history of trauma. However, other studies have found no significant difference in OCD severity between individuals with and without childhood trauma. Further research is needed to clarify this relationship and determine the potential predictors of OCD severity among individuals with a history of childhood trauma.
How Does Childhood Trauma Relate to Comorbidities with OCD?
OCD is often accompanied by other psychiatric comorbidities, such as depression and anxiety disorders. Similarly, individuals who have experienced childhood trauma may be at increased risk for developing various mental health conditions. Some studies have suggested a higher prevalence of comorbid mental health disorders in individuals with both OCD and a history of childhood trauma.
Understanding the relationship between childhood trauma, OCD, and comorbidities can help inform treatment strategies and interventions for individuals with trauma-related OCD.
What are the Potential Factors Influencing the Relationship Between Childhood Trauma and OCD?
Several factors may influence the relationship between childhood trauma and OCD. These factors can include the type and severity of trauma experienced, the age at which the trauma occurred, the individual’s coping mechanisms, and their support systems. Additionally, genetic and environmental factors may also play a role in determining the impact of childhood trauma on the development and severity of OCD.
Is There a Conclusive Link Between Childhood Trauma and OCD?
While there is evidence suggesting a potential link between childhood trauma and the development of OCD, further research is needed to fully understand the nature of this relationship. The current literature provides valuable insights into the topic, with studies exploring the prevalence of childhood trauma among individuals with OCD, the potential impact of trauma on OCD severity, and the comorbidity of childhood trauma and OCD. By addressing childhood trauma as part of OCD treatment, individuals can work towards managing their symptoms and improving their overall well-being.

