Transcranial magnetic stimulation (TMS) is a cutting-edge, non-invasive therapy that uses magnetic pulses to boost brain function. Initially approved for conditions like depression, it’s now showing promise in speeding up stroke recovery. In this article, we will explore the science behind TMS and stroke, including how it works and the evidence supporting its use.
Key Takeaways
- TMS, particularly repetitive TMS (rTMS), may accelerate and enhance stroke recovery by modulating brain activity, neurotransmitters, and immune responses.
- Studies show that rTMS can improve motor skills, balance, and language abilities in stroke patients compared to standard rehabilitation alone.
- TMS works by promoting neuroplasticity, restoring balance between brain hemispheres, and supporting the brain’s healing processes after a stroke.
- Candidates for TMS include stroke survivors with persistent neurological deficits, though it is not suitable for individuals with certain implants, seizure history, or during pregnancy.
- While promising, TMS is considered an adjunct to, not a replacement for, traditional rehabilitation therapies.
What is TMS?
TMS is a non-invasive procedure that uses magnetic fields to influence the activity of nerve cells in specific parts of the brain. A specially designed electromagnetic coil is placed against the scalp and emits brief, focused pulses of magnetic energy. These pulses pass through the skull and induce small electrical currents in the target brain regions. Depending on the type of pulse, TMS can either increase or decrease electrical activity in target brain regions.
TMS is approved by the FDA for depression, obsessive-compulsive disorder (OCD), migraines, and substance abuse disorders. It can also be used off-label to treat other indications, such as stroke. Off-label is when doctors prescribe a treatment for a condition for which it hasn’t been approved, but there is strong evidence to support its use in that condition.
Repetitive TMS, or rTMS, is the most commonly used TMS administration when it comes to psychiatric care, including stroke recovery. This method involves delivering a series of pulses in succession and multiple treatments over a given amount of time.
Limitations in Stroke Treatment
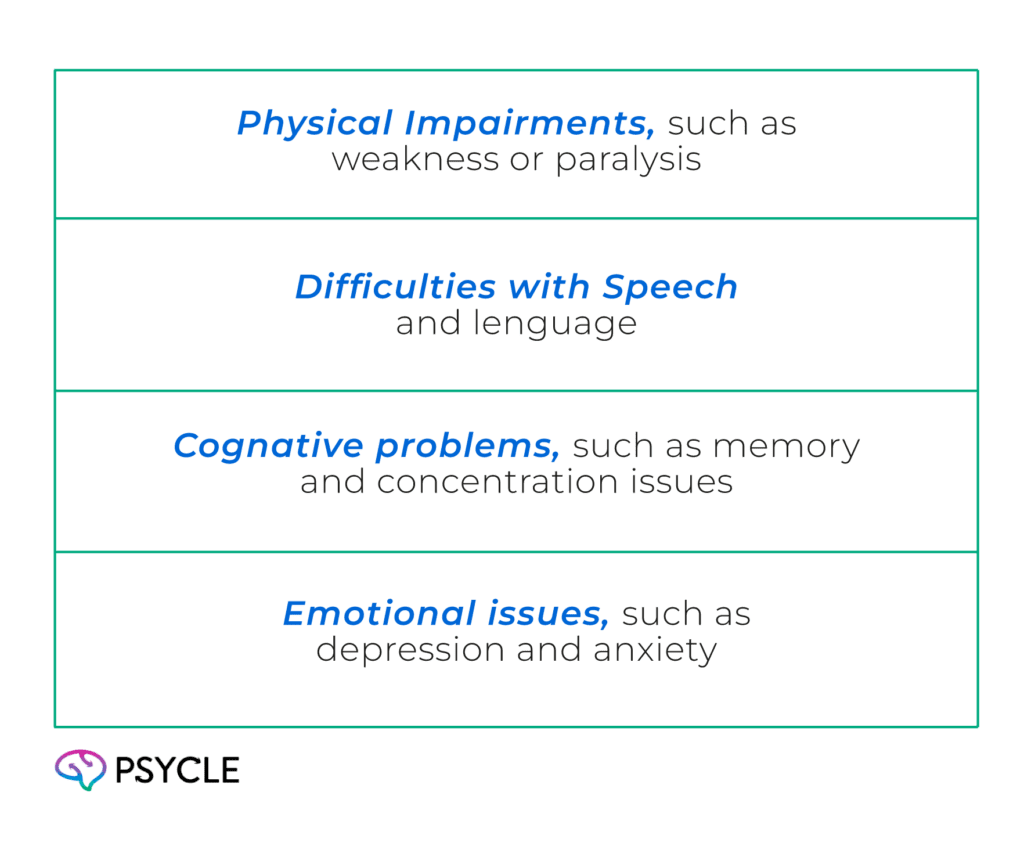
A stroke occurs when blood flow to part of the brain is interrupted or severely reduced, depriving brain tissue of oxygen and nutrients. This causes brain cells to die, leading to neurological deficits, including:
Rehabilitation after a stroke is all about helping patients relearn functions that have become impaired. Through physical, occupational, and speech therapy, rehabilitation helps restore skills for daily living in patients who have had a stroke. It includes activities such as movement and memory exercises, as well as problem-solving.
Yet, despite benefits, progress often slows down after the first few months, and therapy can be tiring and time-consuming. RTMS is a promising option to support and speed up recovery from stroke through addressing some of the underlying biology.
How TMS Supports Stroke Recovery
Studies show that rTMS can improve symptoms in people with stroke-related damage. Scientists aren’t completely clear about the mechanisms underlying these benefits, but there are some accepted theories about how rTMS aids stroke recovery.
Release of Neurotransmitters
Neurotransmitters are chemicals in the brain that transmit messages. Stroke is associated with the abnormal release of neurotransmitters, which is thought to contribute to neurological damage and symptoms. By modulating neurotransmitters, rTMS could help restore this impairment.
A study of stroke patients found that rTMS decreased the release of the neurotransmitter GABA in the motor cortex, a brain area responsible for movement. This decrease was associated with improved motor symptoms..
Immune Regulation
After a stroke, the body’s immune system, its natural defense mechanism, is rapidly activated in response to injury. Immune cells are recruited to the damaged area, releasing pro-inflammatory molecules such as cytokines. While this inflammatory response is initially protective, excessive or prolonged inflammation can damage healthy brain tissue and contribute to deterioration. This heightened immune activity typically lasts from two to six weeks but can persist for months in individuals with chronic post-stroke inflammation.
Studies show that rTMS can influence the immune system response through various mechanisms. In a mouse experiment, rTMS decreased the transmission of brain signals that trigger immune system activation following a stroke. The treatment also caused astrocytes (non-neuronal cells in the brain) to shift from an inflammatory to a healing function. A study of stroke patients found a reduction in the concentration of cytokines in their blood samples following rTMS treatment.
Cortical Excitability
After a stroke, the brain’s two hemispheres can become imbalanced. Typically, the undamaged (contralesional) hemisphere becomes overactive, while the damaged (ipsilesional) hemisphere becomes underactive. The overactive hemisphere can send inhibitory signals that suppress activity in the injured side, making it harder for the brain to recover.
Repetitive transcranial magnetic stimulation (rTMS) uses magnetic pulses to either increase or decrease nerve cell activity in the brain. When applied at low frequencies (typically less than 1 Hz) to the contralesional hemisphere, rTMS can reduce cortical excitability. This helps quiet the excessive activity and lessens the inhibitory pressure on the damaged side.
Conversely, high-frequency rTMS (usually at 5 Hz or higher) applied to the ipsilesional hemisphere can boost cortical excitability. This stimulation helps reactivate brain circuits that were affected by the stroke and supports the recovery of lost functions.
Neuroplasticity
Neuroplasticity is the brain’s ability to reorganize and form new connections, and is a key part of recovery from stroke
rTMS has been shown to promote neuroplastic changes by supporting the reorganization of neural networks. The treatment can stimulate the growth of new synapses (connections between nerve cells), which is crucial for rebuilding circuits damaged by a stroke.
Through these mechanisms, rTMS not only aids immediate functional recovery but may also contribute to long-term improvements by expanding the brain’s capacity for learning.
Evidence for the Benefits of TMS After Stroke
TMS and Improved Motor Skills
In a 2024 study, 30 stroke patients were randomly assigned to receive either conventional treatment or conventional treatment plus low-frequency TMS. The TMS group showed greater improvements in walking ability compared to the control group, including faster stride speed, longer stride length, improved hip, knee, and ankle movement, stronger push-off forces during walking, and better balance. These improvements were correlated with changes in electrical activity in their motor cortex.
In another study, 60 stroke patients were randomly assigned to receive either standard treatment (motor relearning therapy and cognitive rehabilitation) or standard treatment with rTMS. After 4 weeks, the group that received rTMS showed greater improvements in motor function, including lower limb movement and balance, and reduced limb spasticity.
TMS and Improved Language and Cognition
Post-stroke aphasia (PSA) is a language disorder in which stroke damages parts of the brain responsible for speech. In a study of 96 patients with PSA, half of the group received standard speech rehabilitation alone, and the other half had rehabilitation combined with rTMS. The rTMS group had greater improvement in language ability, cognitive function, daily communication, and daily living skills at the end of the four-week treatment.
Who Should Consider TMS?
Repetitive transcranial magnetic stimulation (rTMS) may be a promising option for stroke survivors who experience slow recovery or have chronic neurological deficits despite undergoing standard rehabilitation therapies. This includes patients with persistent motor weakness, walking difficulties, or speech impairments that have not fully responded to conventional treatment.
However, not everyone is a suitable candidate for TMS. Contraindications include the presence of implanted metallic or electronic devices (such as pacemakers, cochlear implants, or deep brain stimulators), a history of seizures or epilepsy, and pregnancy, due to potential risks associated with TMS.
The Future of TMS in Stroke Rehabilitation
Research into TMS for stroke recovery is continuing to grow. Ongoing clinical trials are exploring how different stimulation protocols, timing, and combinations with other therapies, along with TMS, can optimize patient outcomes. Scientists are also using TMS to investigate how biomarkers, such as brain imaging and electrophysiological measures, can predict which treatments are most effective for patients.
While there is growing optimism about TMS as a tool for enhancing stroke rehabilitation, the medical community remains cautiously optimistic. Experts agree that TMS is not a standalone cure but can serve as a powerful adjunct to traditional rehabilitation approaches, such as physical therapy, occupational therapy, and speech therapy.