Traditional antidepressants, such as SSRIs and SNRIs, are commonly prescribed but have significant limitations, prompting the exploration of alternative treatments like ketamine and its derivative, esketamine, which offer new hope for those with treatment-resistant depression.
Traditional antidepressants, such as SSRIs and SNRIs, are commonly prescribed but have significant limitations, prompting the exploration of alternative treatments like ketamine and its derivative, esketamine, which offer new hope for those with treatment-resistant depression.
Key Takeaways
- SSRIs and SNRIs are effective in only 60-70% of patients, and the theory that low serotonin levels cause depression lacks significant evidence.
- Ketamine offers quick relief from depressive symptoms, often within hours, and is particularly effective for treatment-resistant depression.
- Esketamine is FDA-approved for treatment-resistant depression and can be administered intranasally, providing convenience and fewer dissociative effects. However, it may be less efficacious than racemic ketamine.
- Ketamine’s success has highlighted the importance of alternative pathways like the glutamatergic system and mTOR signaling, prompting a shift in depression research and treatment strategies.
The Need for New Antidepressants
Global depression is a growing public health crisis. More than one-sixth of US adults have depression, according to a report from Gallup, which is a nearly 10% higher prevalence than recorded in 2015.
Depression is typically treated using a combination of talk therapy and antidepressant medications. The most common are serotonin and noradrenaline reuptake inhibitors (SNRIs) or selective serotonin reuptake inhibitors (SSRIs).
Yet, despite their widespread use, research shows these medications are only effective in 60-70% of patients.
SNRIs and SSRIs work mechanistically by increasing serotonin levels, a neurotransmitter, in the brain. However, the theory of low serotonin in depression has been heavily criticized, with no significant evidence to support a relationship between serotonin and depression.
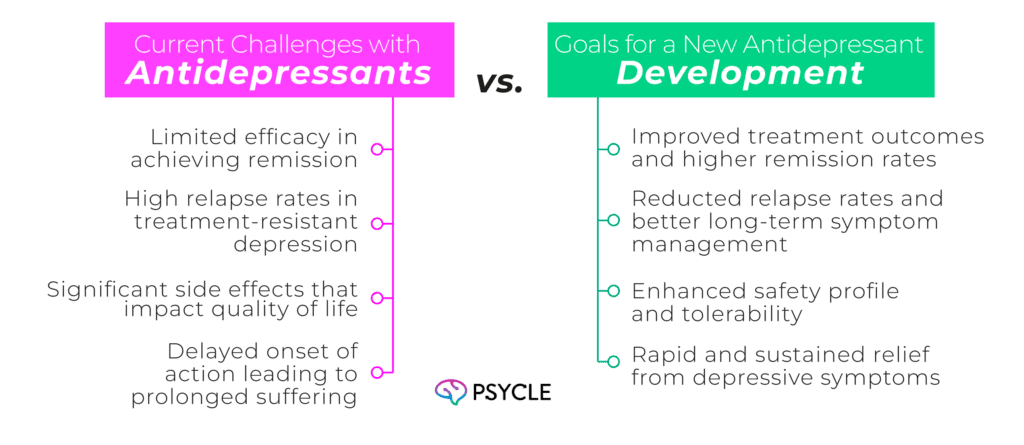
Moreover, studies show that prolonged antidepressant use may actually decrease overall serotonin, potentially causing more harm than good when used over a long period of time.
Antidepressant side effects also deter many patients from using them. The most common side effects are:
- Drowsiness and fatigue
- Gastrointestinal side effects such as nausea
- Sexual dysfunction
- Weight gain
The lack of effectiveness and side effect profile has encouraged researchers to develop and consider new antidepressant treatments over recent years. These have included new medications, such as Brexanalone, the repurposing of ketamine, an anesthetic, and the use of Scheduled psychedelic compounds.
Ketamine as a Treatment Option: The Effectiveness of Ketamine
In the year 2000, Berman et al. conducted the first human clinical study to show the antidepressant effects of ketamine in patients. Antidepressant effects were achieved within four hours of the infusion, and the effectiveness was robust compared to a placebo.
This study encouraged a subsequent double-blind clinical trial that showed ketamine had an antidepressant effect in patients who had previously failed to respond to conventional medication. The antidepressant effects took two hours to onset and were maintained for at least one week in 35% of patients.
Numerous studies since have replicated these findings, and ketamine has become increasingly used as an off-label treatment for depression.
Ketamine is typically provided in two models. One is the clinical model, where patients are given numerous low doses of intravenous ketamine over the course of several weeks and are monitored by healthcare professionals to ensure patient safety.
The other is in ketamine-assisted therapy (KAT), where higher doses are used to induce an altered state of consciousness aimed at facilitating insight and psychological breakthroughs.
In KAT, ketamine is provided in the company of a trained therapist who will meet with the patient in multiple sessions outside of the experience to work through psychological material and help improve patient well-being.
Ketamine vs. Antidepressants
Efficacy Comparison
Multiple studies show ketamine can have antidepressant effects in patients who don’t respond to typical antidepressants. Over 55% of patients with treatment-resistant depression had clinically significant symptom improvement after 3 weeks of ketamine infusion in one study.
In another study, 336 adults with treatment-resistant depression were randomly assigned to receive either quetiapine or intranasal ketamine (esketamine) alongside the antidepressants they were already receiving.
Quetiapine is an antipsychotic sometimes used to boost antidepressant effects in treatment-resistant patients. At the study’s end, 27% of patients taking esketamine were largely symptom-free, compared to 17.6% in the quetiapine group.
However, despite these studies, ketamine may not always be the most effective option. It’s possible some patients may respond better to conventional antidepressant medications than ketamine, so it’s always worthwhile considering multiple options when thinking about mental health treatment.
Side Effects Comparison
Both antidepressants and ketamine have short and long-term side effects. However, the type and nature of the effects are markedly different.
Ketamine and antidepressants have overlapping short-term effects that include nausea, headaches, dizziness, and drowsiness. Ketamine’s short-term effects tend to be more immediate and intense but wear off in the hours after treatment. Antidepressant short-term effects tend to be more mild but take longer to subside.
Ketamine additionally has short-term psychological side effects associated with its dissociative qualities. Dissociation is characterized by the feeling of being outside of one’s body and a lack of awareness of time and space.
Though dissociation can be pleasurable for some and is sought after for recreational use, it can be disorientating and unpleasant for others.
In the long term, side effects associated with antidepressants include weight gain, emotional blunting, sexual dysfunction, and increased risk of cardiovascular disease and diabetes. There is also a risk of withdrawal symptoms or discontinuation syndrome if the medication is stopped abruptly.
Long-term side effects of esketamine, which is administered in small doses, include anxiousness and low energy. Unlike antidepressants, it isn’t associated with withdrawal symptoms and sexual dysfunction has been reported in less than 2% of patients in clinical trials.
KAT involves an infrequent number of high-dose ketamine infusions, and so the long-term physical risks are relatively low. However, ketamine has an abuse potential, and chronic use of high doses can lead to bladder problems, liver damage, memory issues, and potential cognitive impairments.
Onset Time Comparison
The time between an intravenous ketamine dose and antidepressant effects ranges from between 2-100 minutes following a single or course of injections. For esketamine, this value is around four hours following a single course of insufflated doses.
On the other hand, SSRIs and SNRIs may take two to four weeks before any antidepressant effects are noticed.
The Neuroscience of Ketamine’s Action
Depression is a multi-faceted disorder with many psychological and biological factors at play. Researchers don’t know exactly the underlying mechanisms of ketamine’s antidepressant effects. However, there are some accepted theories of action, which include:
- NMDA Receptor Antagonism: Ketamine blocks NMDA receptors in the brain, which respond to the neurotransmitter glutamate. Through blocking inhibitory NMDA-mediated pathways, ketamine can increase glutamate release. This, in turn, may activate brain networks associated with mood regulation.
- AMPA Receptor Activation: AMPA is another receptor that responds to glutamate and is thought to be involved in depression. Ketamine increases AMPA activation by increasing glutamate concentration.
- Increased BDNF (Brain-Derived Neurotrophic Factor): Ketamine increases BDNF levels by activating AMPA. BDNF is a protein that supports neurons’ survival, growth, and differentiation. Elevated BDNF levels are associated with improved mood and cognitive function.
- mTOR Pathway Activation: Ketamine activates the mTOR signaling pathway, crucial for protein synthesis, whic may help overcome brain-related damage associated with depression. mTOR signaling is also associated with synaptic plasticity, the basis for learning and memory, and so increasing this process could increase someone’s ability to learn new healthy thoughts and behavior patterns.
- Reduction of Inflammation: Ketamine has anti-inflammatory properties, reducing the production of pro-inflammatory cytokines. Chronic inflammation is linked to depression, and reducing it can alleviate depressive symptoms.
- Inhibition of Default Mode Network (DMN): Ketamine reduces the activity of the DMN, a network of brain regions typically more active during rest and self-referential thinking. Overactivity of the DMN is linked to rumination and negative thinking patterns common in depression.
Ketamine’s Role in Broadening the Understanding of Depression
Traditional antidepressants primarily target monoamine neurotransmitters, such as serotonin and noradrenaline, and often take weeks to exert their effects.
On the other hand, ketamine works rapidly by modulating the glutamatergic system. Its efficacy has highlighted the importance of glutamate, NMDA receptors, and mTOR signaling in the neurobiology of mood disorders.
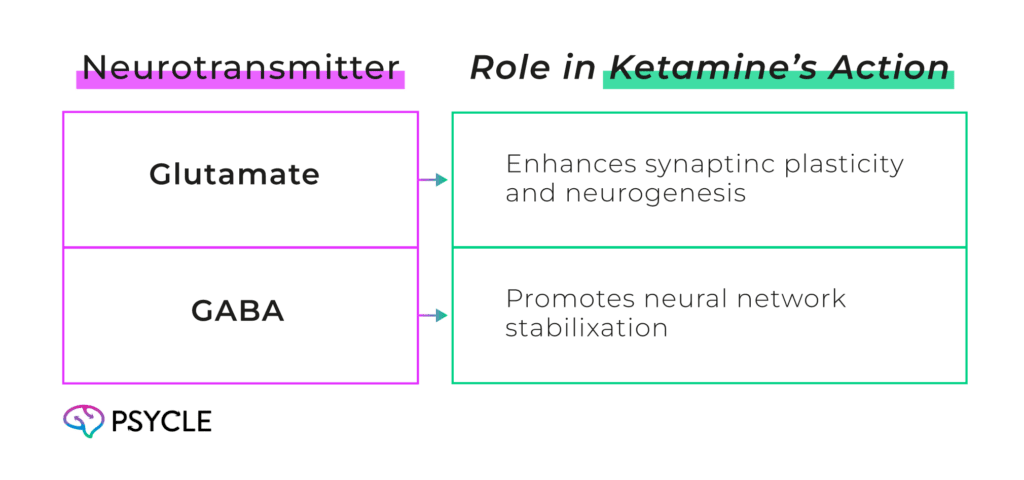
By illuminating these alternative pathways, ketamine has prompted a paradigm shift in depression research, which has historically focused primarily on monoamine targets. This broadened understanding opens avenues for novel treatments.
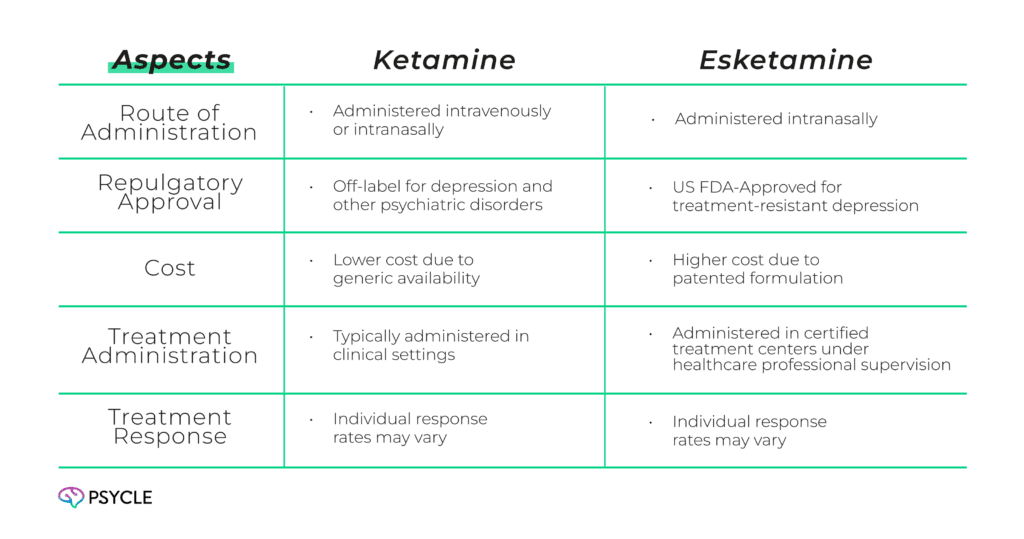
Comparing Ketamine and Esketamine
Ketamine is a racemic mixture containing equal parts of two enantiomers, R-ketamine and S-ketamine. Esketamine (S-ketamine) is derived from this mixture, consisting solely of the S-enantiomer.
It is up to four times more potent than the racemic mix, allowing for smaller doses and decreasing the chance of dissociative effects. It can also be delivered intranasally, which makes it more convenient and less invasive than the racemic mixture.
Whereas racemic ketamine can only be used as an off-label mental health treatment, esketamine is approved by the FDA for treatment-resistant depression and major depressive disorder with suicidality.
Esketamine is generally more convenient to access as a depression treatment. However, a review of several studies showed it may be less effective at reducing depression symptoms and preventing relapse.
Optimizing Ketamine Treatment
Optimizing ketamine treatment for depression involves tailoring the administration, dosage, and frequency to maximize therapeutic benefits while minimizing adverse effects. Clinicians must consider individual patient factors, such as the severity of depression, previous treatment responses, and comorbid conditions, to personalize treatment plans.
Conclusion
Addressing the limitations of current antidepressants is crucial, and novel treatments like ketamine and esketamine provide promising alternatives. Optimizing these therapies can lead to more effective and personalized depression care.
FAQs
What Are the Side Effects of Ketamine Compared to Antidepressants?
There are several overlaps. Ketamine may cause dissociation, which is a feeling of detachment from oneself or one’s surroundings. Antidepressants, on the other hand, are known to have side effects like weight gain and fatigue.
How Does Ketamine’s Action in the Brain Contribute to Its Antidepressant Effects?
Ketamine acts as an open channel blocker on the N-Methyl-D-Aspartate (NMDA) receptors in the brain, leading to synaptic and circuit changes that contribute to its rapid action as an antidepressant.
Why Is There a Need for New Antidepressants?
Despite ongoing development of antidepressants over the past 60 years, mood disorders, especially treatment-resistant depression, continue to be highly disabling conditions. Only a fraction of depressed patients achieve remission with initial antidepressant treatment, and relapse rates are high among those with treatment-resistant symptoms.
How Has Ketamine Challenged the Understanding of Depression?
Ketamine’s discovery as an effective antidepressant has challenged the monoamine hypothesis of depression and led to a broader understanding of the role of other signaling mechanisms, such as glutamate and GABA, in the biology of mood disorders.
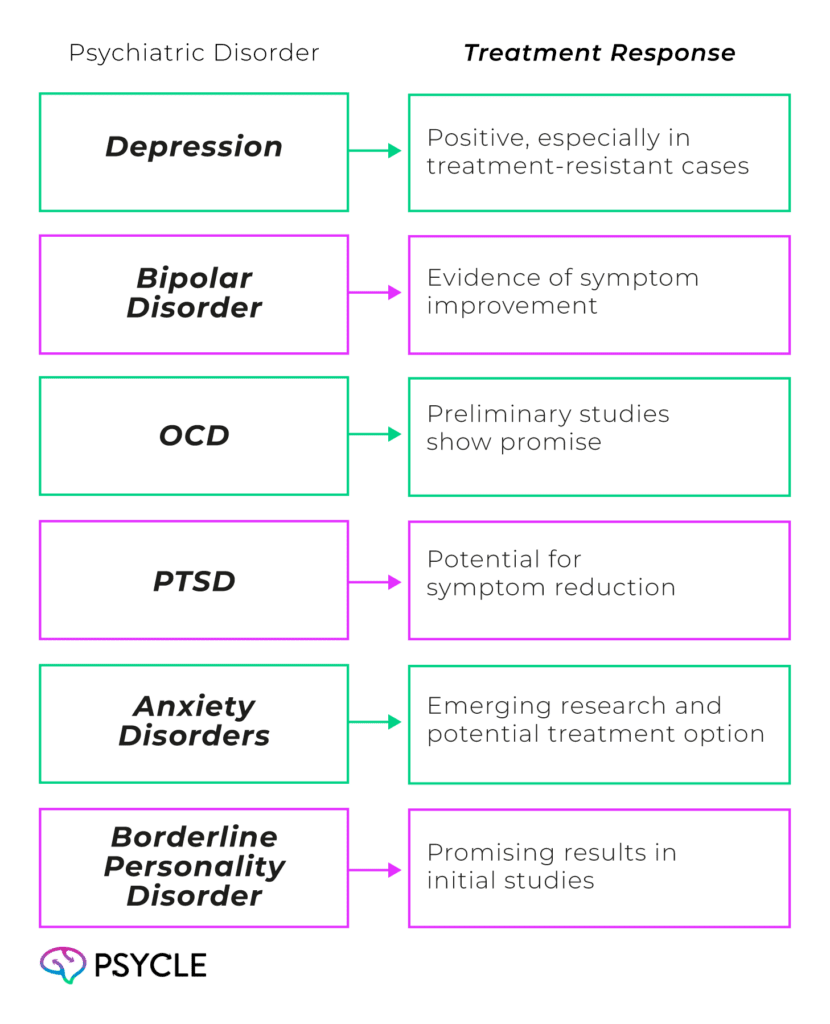
What Psychiatric Disorders Can Ketamine Be Used to Treat?
Ketamine has shown efficacy and safety in treating depression, bipolar disorder, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD). Its use is also being explored in other conditions, such as anxiety disorders and borderline personality disorders.