In recent years, something remarkable has been happening in mental health. Many substances still dismissed by the drug policies of the Global North as having “no medical use”, psilocybin, ketamine, MDMA, LSD, 2-CB, DMT, ayahuasca, mescaline, iboga, and ibogaine, are being spotlighted for their profound healing potential in scientific research.
Centers including Johns Hopkins, NYU, Exeter, and Imperial College are studying how psychedelics work as medicines that can relieve anxiety, depression, PTSD, and addiction. As mental health treatments, psychedelics are especially promising where traditional options fall short.
Key Takeaways
- There is a growing acceptance of psychedelics like psilocybin, MDMA, and ketamine, which are being researched for their potential to treat mental health conditions such as anxiety, depression, PTSD, and addiction, challenging traditional drug policies.
- Psychedelic-assisted therapy combines the use of psychedelics with psychological support before, during, and after the experience, aiming to shift perspectives and promote lasting change through the integration of insights gained during sessions.
- Psychedelics have shown promise in alleviating symptoms of anxiety and depression, with substances like psilocybin and MDMA demonstrating significant benefits in clinical trials.
- MDMA-assisted therapy has shown remarkable results in reducing PTSD symptoms, providing trauma survivors a unique way to confront their experiences without overwhelming distress.
Psychedelics Offer New Hope
This isn’t just a scientific renaissance. It’s also a time of recognising traditional uses of plant-based psychedelics within many Indigenous cultures. Ayahuasca (South and Central America), peyote (Mexico and the United States), and iboga (West Africa) ceremonies increasingly attract people seeking wellbeing beyond Western healthcare. Including combat veterans finding lasting relief after Shipibo ayahuasca ceremonies from treatment-resistant PTSD.
These breakthroughs invite profound questions about our expectations of medicine and mental health. With the flourishing of psychedelic research, mental health can become less about controlling symptoms and more about rediscovering meaning, reengaging with memory, and finding the courage to change.
What Is Psychedelic-Assisted Therapy (PAT)?
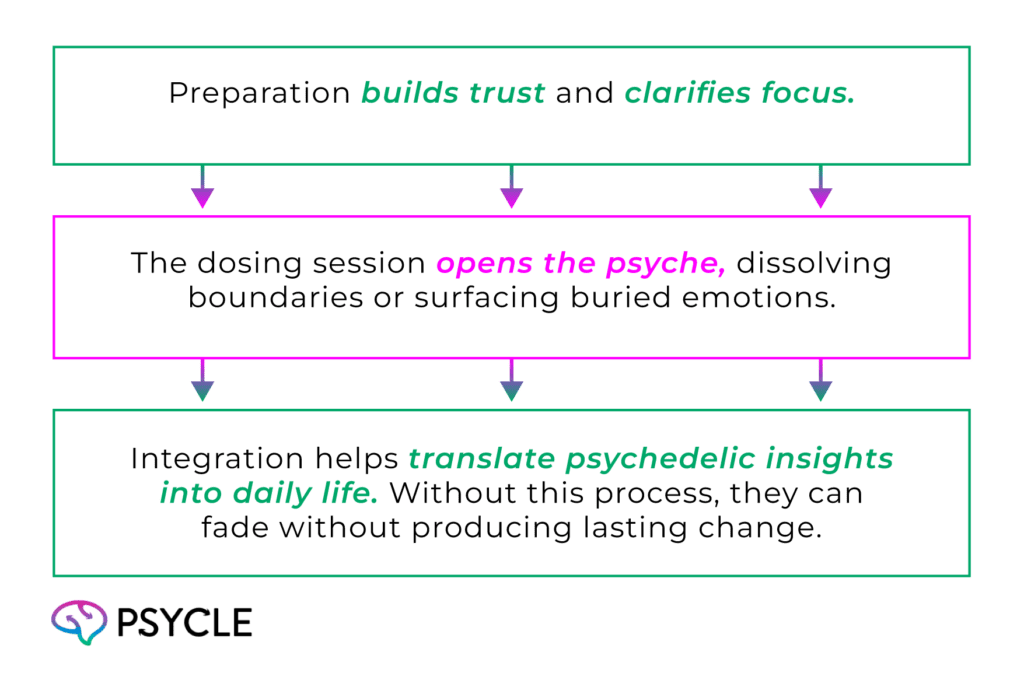
Psychedelic-assisted therapy (PAT) combines the use of a psychedelic compound with psychological support before, during, and after the experience. The goal isn’t to escape reality but to approach it differently: encountering patterns, memories, and emotions from a broader, more compassionate perspective.
Various substances explored within PAT serve different purposes: psilocybin and LSD both tend to invite introspection that can help shift established thought patterns, which can interrupt addiction. MDMA fosters empathy and emotional repair, especially helpful in trauma processing. Ketamine offers rapid relief from depression and can also be used to treat anxiety, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD).
PAT’s power lies in the interactions between medicine, mindset, and the broader context, which is why personalised preparation and aftercare are vital.
Anxiety and Psychedelic Interventions
For those living with persistent anxiety, time often feels fraught with looping thoughts, a racing heart, or a constant background hum of dread. Psychedelics can interrupt that rhythm.
In clinical trials, psilocybin has helped people facing existential anxiety at the end of life find peace. LSD once showed similar promise in 1960s hospice studies, and modern research is revisiting that work. Even short-acting compounds like DMT have shown early potential to ease anxiety through emotional release and a renewed sense of connection.
MDMA, although not a classic psychedelic, reduces social anxiety in small studies with autistic adults. The common thread isn’t chemical sedation; it’s emotional openness. Participants describe feeling safe enough to face what they’ve been avoiding.
Depression and Psychedelic Treatments
Depression can flatten colour, meaning, and joy from life. For many people, antidepressants help, but for millions, they don’t. This is where psychedelics are beginning to shift the landscape.
Psilocybin has been granted “Breakthrough Therapy” designation by the FDA for major depressive disorder. Early trials show that one or two supportive sessions can dramatically reduce symptoms, sometimes for months. Ketamine, and its medical cousin, esketamine, are already legal in many clinics, offering rapid relief through different but overlapping brain pathways.
The working theory is that psychedelics “reset” patterns of thought by increasing neuroplasticity and loosening the brain’s rigid predictive loops. People often describe it less like taking a drug and more like “remembering what it feels like to be alive.”
Still, psychedelics aren’t quick fixes. The positive effects that psychedelics can have on mental health depend on how we approach the experience and what we do to take its realisations forward into the rest of our lives. That’s where therapy, reflection, and community matter most.
Post-Traumatic Stress Disorder (PTSD) and Psychedelics
Few conditions test the limits of psychiatry like PTSD. For many trauma survivors, talk therapy alone can reopen wounds without bringing resolution. MDMA-assisted therapy offers something different: a way to revisit trauma without the complete physiological terror.
In significant Phase 3 trials, MDMA combined with psychotherapy reduced PTSD symptoms so dramatically that regulators are reviewing it for potential approval. Participants often describe a softening, the ability to face memories with compassion rather than collapse.
Psilocybin and ketamine are also under study for trauma-related depression. Ibogaine, synthesised from the West African plant medicine iboga, may help people revisit early traumatic experiences, releasing long-held emotional charges. But ibogaine carries physical risks, so thorough screening and preparation beforehand are crucial for safety, including avoiding certain foods and medications.
Psychedelic experiences don’t delete trauma. Instead, they can create a space where it can finally transform.
Substance-Use Disorders and Psychedelic Approaches
Addiction recovery is another frontier where psychedelics are reshaping expectations. Traditional models often focus on control and abstinence; psychedelic therapy focuses on meaning and freedom.
Psilocybin-assisted therapy has shown remarkable results in treating alcohol and nicotine dependence. Participants often report a deep sense of insight; not just “I should quit,” but “I want to live differently.” Ibogaine has been used in Western clinics for decades to interrupt opioid withdrawal and catalyse emotional breakthroughs.
Both the Amazonian plant brew ayahuasca and iboga, the sacrament of the Bwiti in Gabon, are traditionally used in community-based settings, where research shows their promise for breaking addictive habits by helping people reconnect to purpose and belonging. Research must respect these traditions, in which ritual is key to healing.
LSD, studied in the 1950s for alcoholism, is also making a comeback in controlled research, with a focus on rekindling meaning, not suppressing cravings.
Obsessive-Compulsive and Eating Disorders
While still early, research is expanding beyond depression and trauma. Small studies using psilocybin have shown reductions in obsessive thoughts and compulsive patterns, sometimes after a single session.
For people with eating disorders, psychedelic-assisted therapy is exploring how these substances might loosen rigid beliefs about the body and control. The results are preliminary but moving; a few participants describe feeling compassion toward themselves for the first time in years.
Mechanisms of Action in Psychedelic Therapy
Underneath these effects lies a fascinating dimension of neuroscience. Classic psychedelics, psilocybin, LSD, DMT, mescaline, primarily activate serotonin 2A receptors, which spark temporary changes in brain connectivity. The “default mode network,” associated with self-focus and rumination, quiets down. New pathways open.
MDMA, technically an empathogen rather than a psychedelic, increases serotonin, dopamine, and oxytocin, helping people feel safety and trust. Ketamine, a dissociative, blocks NMDA receptors, rapidly increasing glutamate signalling and promoting synaptic repair.
Different mechanisms that can all be described as leading to a similar outcome: a temporary rewiring allowing emotional truth to surface. The brain becomes more flexible; the mind, more compassionate.
Safety, Ethics, and Psychedelic Access
It’s essential to stay grounded: these are powerful substances, not panaceas. Without skilled aftercare, “bad trips” can be psychologically destabilising. Psychedelic therapy requires careful screening, preparation, and integration.
There are also ethical layers: informed consent, cultural respect for Indigenous traditions, and caution around commercialisation. Not everyone can access these treatments, and cost remains a barrier in most clinical trials.
Accessibility, equity, and education must grow alongside enthusiasm. The future of psychedelics as mental health treatment options in mainstream medicine depends on safety, not speed.
Future Directions and Research Frontiers
The momentum is undeniable, with esketamine (Spravato) fully approved by the FDA for major depressive disorder, and psilocybin, MDMA, and LSD currently in Phase 3 trials; the final stage. Globally, with clinical trials, the policy landscape is shifting. Oregon’s psilocybin program, Australia’s legal prescription model, and Canada’s compassionate-use exemptions signal a broader change.
New frontiers are emerging: combined approaches (like psilocybin plus somatic therapy), digital integration tools, and community-based healing models. Universities are offering courses on psychedelics in medicine and culture, and therapists worldwide are taking specialised training to work with clients with psychedelics.
Yet the most exciting research question isn’t whether psychedelics work; it’s why. It is finding out how these experiences restore meaning, self-compassion, and connection. And ensuring modern psychiatry respects Indigenous communities when considering plant-derived psychedelics, as much as it values their therapeutic potential.
In the end, psychedelic medicine isn’t about chasing euphoria; it’s about coming home to ourselves. Beneath the chemistry and data lies the possibility of healing through expanded understanding, embodiment, and awe.
Frequently Asked Questions
Which Psychedelic Shows the Most Substantial Evidence So Far?
MDMA for PTSD and psilocybin for depression hold the most advanced data. Both are in Phase 3 trials with a Breakthrough Therapy Designation, granted when preliminary clinical evidence shows a drug may offer a substantial improvement over existing therapies.
Are Psychedelics Safe for Everyone with Mental Health Issues?
No. People with certain conditions, including psychosis, bipolar I disorder, or severe cardiac issues, face a higher risk. Medical supervision and psychological preparation are essential.
How Do Psychedelics Differ from Standard Antidepressants?
Traditional antidepressants manage symptoms over time. Psychedelics can create brief but profound experiences that can transform perception and emotion, often with lasting impact after just one or two sessions.
Sources
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5773453/
- https://pubmed.ncbi.nlm.nih.gov/37844352/
- https://www.fdli.org/2025/03/from-secret-tests-to-therapy-trials-mdmas-long-road-to-legitimacy/
- https://psychedelicalpha.com/data/psychedelic-drug-development-tracker
- https://www.sciencedirect.com/science/article/pii/S2666459325001052
- https://www.hopkinsmedicine.org/health/wellness-and-prevention/why-arent-my-antidepressants-working
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5603818/
- https://www.onaya.io/onayas-story
- https://www.science.org/doi/10.1126/science.adf0435
- https://academic.oup.com/nc/article/2023/1/niad017/7220654
- https://pubmed.ncbi.nlm.nih.gov/36844020/
- https://www.youtube.com/watch?v=z7OnZtvPm84
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5641975/
- https://www.youtube.com/watch?v=4RZ8t92S65M
- https://ibogaineguidelines.com/clinical-guidelines/introduction/
- https://www.nature.com/articles/s41591-023-02565-4
- https://www.nature.com/articles/s41386-023-01629-w
- https://publichealth.jhu.edu/2025/mental-health-crisis-hits-nearly-1-in-10-us-adults
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2997873/
- https://pubmed.ncbi.nlm.nih.gov/39515264/

