When someone faces a severe mental health disorder that doesn’t improve with traditional therapies, doctors may recommend brain stimulation treatments. Two of the most well-known options are Transcranial Magnetic Stimulation (TMS) and Electroconvulsive Therapy (ECT). Both can provide relief when other treatments fall short, but they work in very different ways and have distinct histories.
In this article, we’ll explore the background, science, and treatment process of both TMS and ECT. We’ll also look at who might benefit from each, their side effects, and things to consider if you or a loved one is exploring these options.
Key Takeaways
- ECT and TMS are both effective mental health treatments, but ECT often works faster and is better suited for severe or urgent cases
- TMS uses magnetic pulses to stimulate targeted brain regions without anesthesia or seizures, whereas ECT uses controlled electrical currents to induce a monitored seizure under anesthesia.
- TMS side effects are usually mild and temporary, while ECT’s effects are more severe and can include long-term cognitive damage.
- The choice between ECT and TMS depends on your condition, symptom severity, urgency of relief, prior treatment history, and whether or not anesthesia would be safe for you.
What is ECT?
Electroconvulsive therapy (ECT) involves sending electrical currents through the brain to induce a seizure (a sudden burst of electrical activity). The basic idea is that causing a controlled seizure can reset the brain’s electrical activity, restoring nerve circuits that are dysfunctional in mental health disorders.
ECT was first used in the 1930s as a way to treat severe mental health disorders, particularly schizophrenia. At the time, mental health care had few effective treatments, and ECT quickly became widespread.
Although it proved effective, the popularity of ECT declined with the introduction of less invasive and risky psychiatric medications. Misuse of ECT in mental hospitals also gave the treatment a bad reputation.
However, ECT continues to be used today. For patients who don’t respond to antidepressants, ECT remains one of the most effective treatments. It also remains a first-line treatment for bipolar disorder with catatonia, where patients experience abnormal movement during manic episodes.
How Does ECT Work?
During ECT, you’ll be put under general anesthesia and given medication to relax your muscles. Electrodes are then placed on your scalp, and a carefully controlled electrical current passes through the brain. This current triggers a brief seizure, usually lasting less than a minute. While this may sound alarming, the seizure is closely monitored and controlled to minimize risks.
A typical course of ECT involves 6 to 12 treatment sessions, typically administered twice a week.
During ECT, the seizures cause widespread changes in brain activity and chemistry, influencing how brain areas interact with one another. The treatment has a sustained effect on levels of neurotransmitters, which are chemical messengers that send signals throughout the brain.
In addition, ECT increases measures of neuroplasticity, the ability of brain cells to grow and form new connections. Neuroplasticity helps repair damage to nerve circuits and potentially “resets” pathways associated with mental health disorders.
What is TMS?
TMS is a non-invasive treatment that uses magnetic pulses to stimulate electrical activity in specific brain areas. TMS emerged as a promising alternative to ECT because it does not require anesthesia or induce seizures. Instead, TMS uses a magnetic coil placed on the scalp to send brief magnetic pulses into specific parts of the brain.
The area of the brain most commonly targeted by TMS for depression is called the dorsolateral prefrontal cortex (DLPFC). This region plays a critical role in regulating mood, decision-making, and emotional control. In many people with depression, the DLPFC is underactive.
TMS first appeared in the 1980s when scientists discovered that magnetic fields could safely and non-invasively stimulate nerve cells in the brain. However, it wasn’t till 2008 when the FDA approved TMS for treating treatment-resistant depression (TRD). It has since received approval for headache disorders, OCD, and quitting smoking, and continues to be used “off-label” for treating various other mental health disorders.
How Does TMS Work?
During a TMS session, you’ll sit comfortably while a technician places a magnetic coil on your scalp over the targeted brain region. The machine then sends short bursts of magnetic pulses, each lasting a fraction of a second.
A typical TMS session lasts around 30 to 40 minutes. Since no anesthesia is used, you’ll remain awake and alert throughout the treatment and can resume normal activities immediately afterward. Treatment usually involves daily sessions, five days a week, for four to six weeks.
Scientists think this repeated stimulation helps restore balanced communication across the brain. Studies show that, like ECT, TMS increases measures of neuroplasticity and affects neurotransmitters. TMS particularly affects monoamine neurotransmitters, which play essential roles in mood, motivation, and energy.
Comparing the Effectiveness of ECT and TMS
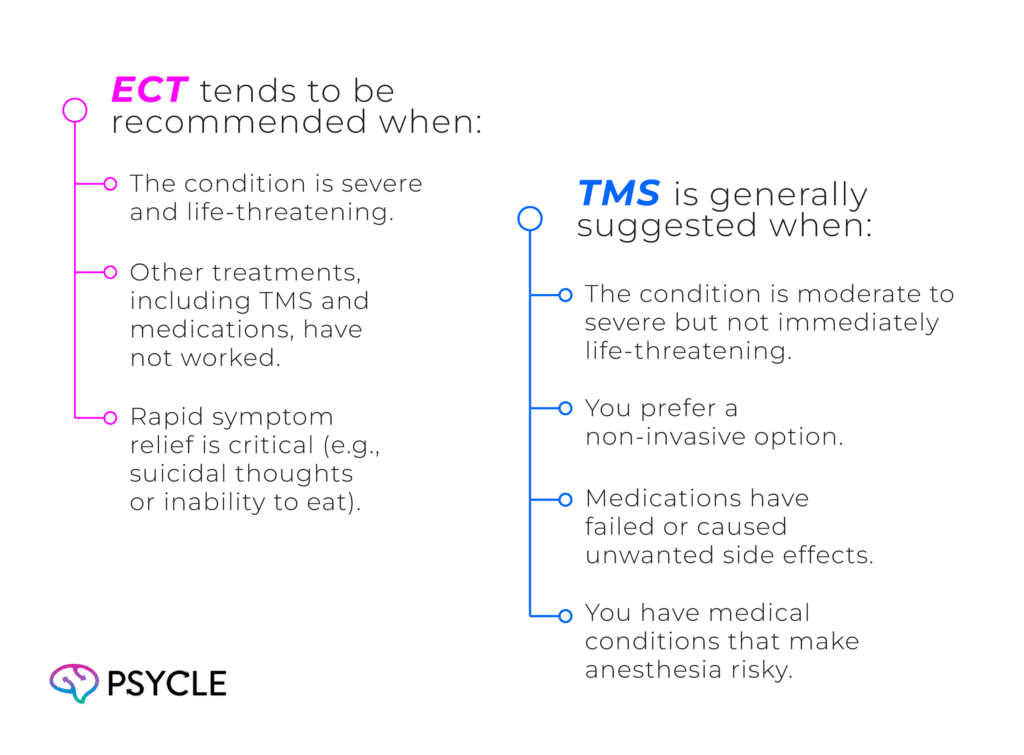
Both TMS and ECT have substantial research supporting their effectiveness, but their uses differ depending on the severity of depression and patient needs.
Clinical studies show that ECT is effective for around 58 to 70% of people with TRD, while TMS is effective in around 50% to 60%. ECT also tends to produce improvements within a few sessions, whereas TMS can take several weeks.
As such, ECT may be best suited for someone with severe TRD in urgent need of relief, such as those at-risk of suicide. However, TMS is often preferred because it’s less invasive and has fewer risks.
There’s less research on the effectiveness of TMS and ECT for other mood disorders. However, clinical trials suggest TMS can be beneficial for conditions such as anxiety and PTSD, and is a preferred option in these cases.
ECT, on the other hand, is often more effective for psychotic disorders like schizophrenia, where there’s stronger clinical evidence to support its use.
Side Effects and Safety Considerations
One of the reasons TMS has gained popularity is its safety profile. Because it doesn’t require anesthesia and targets only specific brain regions, most people tolerate it well. Side effects are usually mild and short-lived. They include:
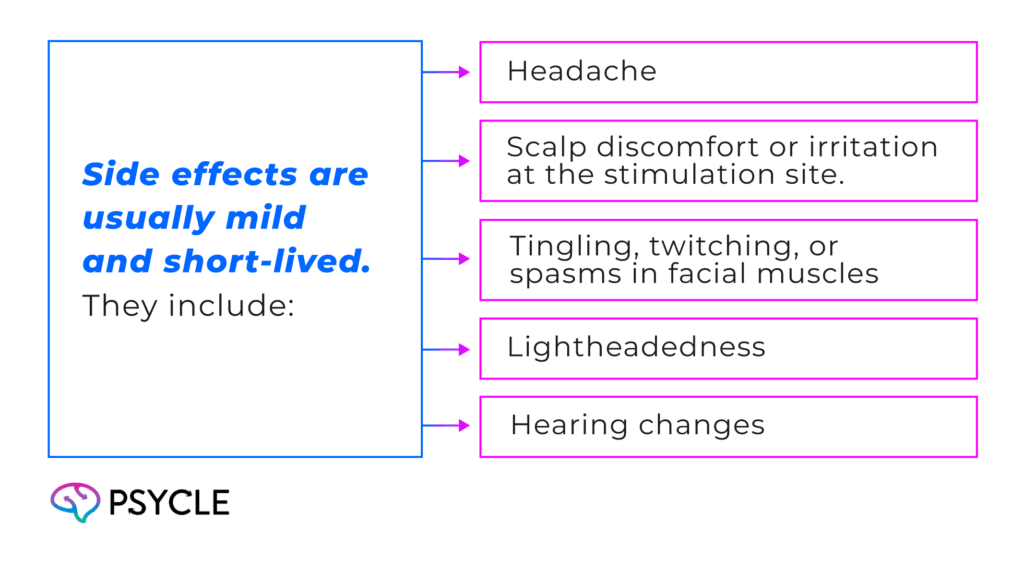
TMS has been known to induce seizures and mania. However, these severe side effects are infrequent.
ECT, on the other hand, involves more risks. Anesthesia carries its own set of dangers, especially for older adults or people with heart or lung problems. The induced seizures also cause side effects, including:
- Short-term memory loss
- Confusion
- Headaches
- Muscle soreness
- Nausea
Long-term treatment may also lead to long-lasting cognitive impairment, such as memory problems.
Both treatments require careful medical evaluation before starting. A doctor will consider your overall health, other medications, and mental health history to decide which is safer and more suitable.
Who Should Consider ECT or TMS?
If you’re considering TMS or ECT, you’ll want to consider several factors, such as the severity of your mental condition, how quickly you need relief, past treatment history, and medical considerations.
Looking Ahead: The Future of Brain Stimulation
Brain stimulation therapies like TMS and ECT are continuing to evolve. Researchers are exploring new ways to make these treatments more effective, with fewer side effects, and easier to access. There’s also growing interest in combining brain stimulation with psychotherapy and medications to improve outcomes.
Other emerging technologies, such as transcranial direct current stimulation (tDCS) and deep brain stimulation (DBS), are being studied and may provide new hope for people with mental health disorders.
Final Thoughts
Both TMS and ECT are potent tools in the fight against depression, especially when other treatments haven’t worked. ECT offers rapid, often dramatic relief for severe cases but involves anesthesia and a more intense procedure. TMS provides a gentler, non-invasive alternative that can be effective for many people, though it usually takes longer to see results.
If you or someone you love is considering either of these options, it’s essential to get a professional opinion from your healthcare provider. They can advise you on whether you are suitable and which treatment would most benefit your needs.
FAQs
Can ECT Cause Brain Damage?
There’s no strong evidence to suggest that ECT causes long-lasting brain damage, but it can cause lasting cognitive problems. This risk may be caused by changes in how the brain stores and processes information, rather than physical damage.
Which is More Expensive, ECT or TMS?
In most cases, ECT is more expensive per treatment course because it requires anesthesia, medical staff, and a hospital or surgical setting. TMS, while still costly, is usually performed in an outpatient clinic without anesthesia, lowering the overall cost. However, the final price for either treatment depends on factors like location, insurance coverage, and the number of sessions needed.
Sources
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10198476/
- https://psyclehealth.com/alternative-treatments/what-is-transcranial-magnetic-stimulation/
- https://pubmed.ncbi.nlm.nih.gov/38844713/
- https://www.ncbi.nlm.nih.gov/books/NBK538266/
- https://pubmed.ncbi.nlm.nih.gov/33324060/